9. OXYGEN and CARBON DIOXIDE
Oxygen. O2. A colourless, odourless gas forming one fifth of the Earth’s atmosphere; the most abundant element in the Earth’s crust.
Carbon Dioxide. CO2. A colourless, odourless gas, with a slightly acid taste, present in air at around 300 ppm, but variable.
Putney, London
Before I was born I had to get the oxygen that I needed by way of my mother’s lungs and blood stream. It arrived on my side of my placenta at a fairly low pressure, but my haemoglobin was designed to operate efficiently under these conditions. As soon as I was born I yelled loudly and promptly took over the task of obtaining oxygen from the air for myself.
I use this oxygen to burn fuel to produce energy, and in the process, like everybody else in the world, I am a carbon dioxide factory. On the day I was born I produced roughly six gallons[1] of this colourless, odourless gas. I excreted it most efficiently through my newly expanded lungs without my proud mother knowing anything about it.
Ilfracombe, Devon
I liked Ilfracombe, though I didn’t quite understand why we had come there. I knew it was to do with ‘the war’, but I was not really sure what that meant. Ilfracombe was an exciting place, full of things I had never seen before, though the big waves in the sea were rather frightening. Sheila told me that they had been thirty feet high last week and that someone had been drowned. Still Mummy and Auntie Gwen would make sure I was safe, wouldn’t they? Yes, of course they would.
We had been at Auntie Gwen’s house for a month now, and so much had happened. There had been that funny evening when we children had had to take our clothes off and be painted all over with that yellow stuff[1], though I did not know why. I had run around playing while it dried and had tripped on the edge of the carpet. As I had fallen I had knocked against the hot paraffin stove in the middle of the room and had hurt my joey. Mummy had said it would be better in a minute, but Judy had laughed.
Then there was the sweet shop down the road that sold ice-cream cones for a ha’penny. They were very small, but very nice. I liked the strawberry ones best. They also sold sherbet, which came in folded yellow paper packets with tubes made of liquorice sticking out of them. I didn’t like the taste of the liquorice but if you were careful you could suck up the powder without getting the liquorice wet and then you didn’t get the taste of it. The sherbet was lemony and fizzed wonderfully in your mouth.
It was when I was on my way one morning to the little sweet shop that I was stopped by a really big boy whom I had never seen before.
‘Gi’e me money,’ he said, ‘or I’ll gi’e yer iodine.’
I was very puzzled, and quite a bit frightened. The big boy looked fierce and threatening yet the offer of iodine for money seemed fair enough. I had always liked the little glass vials of deep brown liquid that Mummy bought at Woolworth’s to treat cuts and grazes. It looked such powerful medicine, and it was nice to be able to dab a wound with a small piece of cotton wool dipped in iodine and know that you were killing the germs and protecting yourself.
‘Gi’e me money, or I’ll gi’e yer iodine,’ the boy repeated. This time there could be no doubt about the threat in the voice but still I did not understand why.
‘All right,’ I said. I handed over the two ha’pennies and waited. The boy grapped the coins, mumbled something that I couldn’t catch, turned and started to walk away.
‘What about the iodine?’ I said.
The boy turned round. ‘Iodine? I’ll give you iodine.’ But he didn’t. He just walked away.
I burst into tears. It was so unfair. The big boy had cheated me.
‘What is the matter, young man,’ said a kindly voice. I looked up at the lady who was speaking. I wondered where she had come from. She smiled at me. Through my tears I told her about the boy and how he had taken the money but hadn’t given me the iodine. She didn’t seem to understand about the iodine at all.
‘Never mind,’ she said, ‘we’ll go and tell Mrs Jones in the shop. She may know who the boy was.’
We walked down the road to the little shop and told Mrs Jones the tale.
‘That was probably young Billy Porter,’ she said. ‘He was in here a few minutes ago. A rough lad he is. I’ll speak to him next time I see him.’
She laughed when I told her about the iodine.
‘Iodine?’ she said. ‘Iodine?’ She looked puzzled. Then she laughed. ‘ He must have said ‘a hiding’. Yes, of course, that would be it.’
I did not understand at all what she meant but I did not like to ask her to explain.
‘Would you like some sweets?’ she continued. ‘You can pay me later when you get your money back.’
I nodded gratefully and pointed at a packet of sherbet.
On the way home I sucked the delicious powder into my mouth where it was wetted by my saliva and fizzed most satisfactorily. The little bubbles of carbon dioxide sparkled and danced on my tongue.
Leominster, Herefordshire
It was market day. The sun shone brightly and the small town was awash with interesting animals and strange people. The shops were bulging with farmers’ wives and their children, while Corn Square was full their aunts and grannies and cousins. Everywhere I walked there was an air of excitement that set my nerves atingle. I was fascinated by the different smells in the different shops. I particularly liked the husky scent of grain inside the corn seed shop, the smoky bacon taste and the cheesy odour in the grocers, and the smell of new leather in the shoe shop where they had a wonderful machine that let you look at the bones in your feet. Outside in the square there were other smells: of doughnuts cooking, of coffee roasting and of horse manure.
I had a most enjoyable time watching the market traders. There was one man selling knife sharpeners. He was a huge fellow with long hair and spots on his face which made me wonder if he had got a horrible disease. He produced several knives from a suitcase and showed the people watching that they were so blunt that they would not cut his arm when he drew them across his skin.
‘Now watch this,’ he shouted. ‘You just pop the blade of the knife into the sharpener like this and pull it back three or four times, and what have you got? An edge that would chop the whiskers off a cat without it noticing. Look at this and you will see what I mean.’
He held up a sheet of paper by it edge and sliced through it cleanly with one single swipe.
‘There you are. What did I tell you. You’d pay a fortune in the shops but I am giving them away at sixpence each. You can’t ask fairer than that now can you, madam? Who wants one then?’
Several of the ladies stepped forwards and soon money and goods were changing hands. I knew that they would not need one of those at Wilf’s farm for he had a splendid grinding wheel on a frame with a large handle. That would sharpen anything you wanted. Too sharp really; old Uncle Harry could slice the ham so thin that you felt as though you weren’t really getting anything on your plate
I looked at my watch; it was almost ten to one. I was meant to be meeting my mother and Janet and Sheila outside the Talbot at one o’clock. But what was this? A tall dark gypsy was calling a crowd to gather around him.
‘Come here, come here, listen to me. I’ll tell you things that they can’t teach at your schools and your colleges. I’ll show you things that I learnt in the University of Life. I’ve got herbal pills and potions here that will cure your gout and flush your kidneys. What do they know about it, those doctors?’
He paused for a few seconds, as though challenging the crowd to answer. Then he continued
‘ If you have a sore throat, one of them will tell you to soothe it with glycerine; another will give you permanganate to gargle. Let me show you what can happen if you listen to them. Watch this and see what happens if you do as the doctors tell you.’
He held a large potato up for everyone to see.
‘See here, I’ll cut a thin slice out of the middle of this potato, like this, and you can hold it for me, missus.’
He handed the thin round slice of raw potato to an elderly woman at the front of the crowd.
‘We’ll scoop out the middle of the two pieces that we have left, here like this, so that we have two potato cups. Now here is some glycerine,’ and he held a sticky bottle up high for them to see. ‘I’ll pour some of it into this cup here, like this, and put it here on the ground. Now here is some permanganate which I bought at the chemists half an hour ago.’
This time he held up a small twist of paper, which he carefully unfolded so that he could pour the dark purple crystals it contained into the second potato cup.
‘Let’s put the slice of potato onto this cup,’ he said as he retrieved it from the woman and placed it carefully on the cup containing the permanganate crystals. Then he turned the covered potato cup upside down and placed it on top of the cup holding the glycerine.
‘I want you to watch closely. While the two medicines are kept apart everything is all right. But when you let them mix together see what happens.’
He bent down and with the end of his knife he pushed the slice of potato out of its position so that the two cups were no longer separated by it.
‘Step back everybody. Stand back, missus. Come on now’
We all stood back and gawped. What was going to happen? Nothing it seemed. I was just beginning to think it was all a trick when there was a puff of steam (or was it smoke?) and the top of the potato was pushed off and the whole thing went up in spitting bubbles.
‘There now that’s what the doctors will do for you if you let them. My herbal mixture will cure you and keep you well without blowing you up. Who wants a bottle? Only sixpence a bottle. It’s almost giving it away.’
No one moved for a moment, but eventually one lady did buy a bottle of his mixture. Now the ice was broken, others came forward, so that in the next two minutes he sold five or six more bottles.
When we got back to the farm I told Wilf about the gypsy.
‘Glycerine, and permanganate, eh? The vet used some permanganate on my sheep once. He told me that you could make gunpowder out of it; he said it’s because it’s got lots of oxygen in it.’
Gunpowder, eh? That sounded interesting.
Betton, Shropshire
Before we were sent off to bed the School Matron would pour out cocoa for us to drink. It was delicious. Then we had to clean our teeth, and finally had to gargle a weak solution of Dettol. This ritual took place every night of the term and was designed to keep respiratory tract infections at bay.
Though in general we were all fit healthy youngsters there was occasionally a need for one or two of us to miss school and the best trick we had was to pull down an eyelid and rub the white of the eye till it turned red. Matron said this was ‘conjunctivitis’ or something like that, though we usually called it ‘pink eye’ or ‘sticky eye’. It was the signal for immediate isolation and eyedrops every two hours; these stang when they were put in, but the sting soon went away and as long as you kept on rubbing your eye it was certain to keep you in the sick bay for a couple of days. Once I did have the real thing and that was really unpleasant. Matron had to bathe my eyelids in the mornings before I could get them open as they were stuck together with yellow crusts.
Very occasionally we would do the fainting trick. This was splendidly dramatic; you breathed in and out very rapidly for about half a minute, and then you shut your voice box tightly and tried to blow out, but you couldn’t however hard that you tried[1]. Then there was a buzzing in your ears and after a moment or two you passed out.
I only did this a couple of times but it seemed quite interesting at the time. I did not know, of course, that it was a dangerous thing to do. The pressure I built up inside my lungs stopped the blood flowing onwards to my brain, so that it was a lack of oxygen that made me become unconscious.
It is lucky that none of us did ourselves an injury.
Putney, London
‘John, could you make some soda water for me, please?’ asked my father. ‘Uncle Alan is coming and we haven’t got anything to go with the scotch.’
‘Yes, Dad. I’ll do it right away.’
I was thrilled to have the chance of using the beautiful glass syphon with its woven wire covering. It had such an intriguing pattern as the wires ran obliquely in groups of four round the glass dipping under or flying over the other groups as they met creating a series of shiny diamonds where the glass showed through the metal mesh. How safe and cared for it looked in its fine coat of silver armour
I went to the drawer where I knew the ‘Sparklet’ bulbs of carbon dioxide were kept. Good, there was a new packet just waiting to be used. The metal bulbs themselves were a pleasure to handle. Smooth to the touch and as light as a half crown in your hand, yet packed with amazing power when you let the gas out. I loved to watch it bubbling fiercely into the syphon, but I knew that you must go slowly at first, and shake the syphon well, so that the carbon dioxide dissolved in the water keeping the pressure to a safe level. I wondered what would happen if you turned the bulb holder too quickly. Would the glass shatter despite the wire protection? I thought probably not, but I was not brave enough to try. I was fascinated by the way the bulb got so cold as the gas flowed out of it. I wondered why that happened.
I was shaking the syphon vigorously when that the idea came to me. Perhaps I could use the tremendous power in the bulb for jet propulsion. I had heard all about the Whitley Armstrong aeroplanes; surely it would work with a model car too. I would try it out later, when no-one was around. I put one of the unused cylinders in my pocket.
‘I’ve made the soda water, Dad.’
‘Thank you, John.’
It was mid-afternoon before I found myself alone. Mum and Dad were asleep in the sitting room upstairs, their customary Sunday nap, and Janet and Sheila had gone for a wet and windy walk on Putney Common. Now I could take the chance to experiment with the small metal cylinder. I had already sorted out a splendid Lagonda, which was painted the dark green of cooked spinach but was glossy and gleaming like a laurel leaf. It was my favourite Dinky toy. Carefully I tied the Sparklet bulb to the car with string so that it lay lengthways on top with its small sealed nozzle pointing backwards. So far so good. Now it was time to gently file away the soft metal plug that sealed the end. Slowly does it... careful now. I stopped for a moment to see how it was going. The dull rounded end was now shiny and quite flat. I would not be able to file away much more now as there was really very little sticking out beyond the nozzle. Still I would just go as far as I could. That’s it then. Time to get out the penknife. All the years I owned and loved penknives this was the very first time I had found a use for the marline-spike. I knelt on the floor holding the car with my left hand. Slowly I advanced the spike in my right hand. Dare I stick it through what was left of the seal? Yes, of course I did. Here goes then. With a sudden thrust I had done it. There was a tremendous hiss and I jumped back like a startled rabbit. The car shot across the floor at a fantastic speed and smacked hard into the skirting board chipping the paint as it did so. It then flipped over and hissed away for a few more seconds, at the same time writhing like an injured worm. Finally it lay still and silent, its energy sapped, its moment of glory already fading into history. There was a frost on the outside of the cylinder, which began to melt even as I watched. But it had worked, it really had worked. Glancing briefly at the damaged paintwork, I picked up the evidence and quickly left the room.
Epsom, Surrey
I have never forgotten my first chemistry lesson. Before it started I did not really know what chemistry was... something to do with chemicals certainly, but what were they? My mother was always talking about ‘chemicals’ but she had never said exactly why one substance was a chemical while another was not. I had always assumed that it was rather like the way some plants were weeds while others were not. Grown-ups seemed to know which was which, though it was not always so obvious to me.
‘Today I am going to tell you something about oxygen. It is a colourless gas that is present in the air, and we would all die without it. It does not have any smell. It is a highly reactive substance and it supports combustion.’
The teacher paused and looked at a boy in the front row.
‘How much oxygen is there in the air, Perkins?’
‘I don’t know, sir.’
‘Would you like to do an experiment to find out?’
Perkins looked at him dubiously.
‘Perkins is going to carry out an experiment to show us how much oxygen there is in the air. Gather round this table so that you can all see but don’t get too close or you will be in his way. That’s good. Now, Perkins, I want you light this short candle and place it on this piece of cork floating on the water in this basin. Good, that’s splendid.’
He paused for a moment. Then he picked up a large glass jar, which he called a ‘bell jar’. It was rather like the thing they used in cake shops to cover the cakes with, so that wasps could not get at them.
‘Now, Perkins, I want you to place this jar over the top of the candle so that the rim of the jar is in the water and the candle is burning inside the jar. There that’s good.’
We watched in amazement as the level of the water began to rise up inside the jar.
‘Why is it doing that, sir?’
‘Because the flame is using up the oxygen inside the jar. Watch and see what happens.’
Fascinated we watched the water continue to rise and then suddenly the flame went out.
‘Why did that happen, sir?’
‘Because there is no more oxygen left so the wax cannot burn any more. We must wait a few moments for the gas that is left inside to cool down again and then we will measure it and see how much oxygen has been used up. When it burns it makes another gas called carbon dioxide so we must get rid of that too before we can make the measurement. We will add a chemical called sodium hydroxide which will absorb it.’
Later he continued:
‘So you can see, Perkins, one fifth of the air must have been oxygen. Thank you for your help. Now we are going to do another experiment. I have two jars of water here, both filled from the same tap. We are going to boil this one for a few minutes so that the air is all boiled out . That means that there will be no oxygen dissolved in the water. This jar we are going to shake up and thoroughly mix with the air so that there will be plenty of oxygen dissolved in the water. Now we are going to put a nail and then pour a thin layer of oil on top. It will take several days before we see any difference but eventually we will notice that one of the nails goes rusty while the other stays bright. Which nail do you think will be the one to go rusty, Perkins?’
Nobody knew.
Biology was great fun, especially the practical lessons. My mother had bought me a beautiful dissecting set, with scalpels and tweezers and fine sharp scissors, each with its own little pocket in a canvas roll with a string tie to keep it safe. There was also a small glass syringe with a shiny steel plunger for injecting things though I was not sure what sort of things. Still it was very scientific to own a syringe.
‘We are going to dissect the earthworm to-morrow afternoon,’ Toad Ellis said. ‘First we have to dig up some worms and then we will have to kill them. How do you think you can kill an earthworm?’
Nobody knew why he was called ‘Toad’, but the nickname did not imply any lack of respect. We knew he was one of the country’s great experts on snails, indeed he had written a book about them, and we admired him immensely.
‘Poison them, sir,’ said someone.
‘Hit them with a hammer, sir,’ said another.
‘No, neither of those. What you do is boil some water for ten minutes so that all the oxygen has been driven out of it, then let it cool, put it in a jar, pop the worms in and seal the top so no air can get in. If you wait twenty four hours or so the worms will have died from lack of oxygen.’
‘That seems a bit gruesome, sir.’
‘I don’t think its too bad really. They don’t know that they are being starved of oxygen. Worms are not like us, you know.’
‘Why does boiling the water make the oxygen come out of it?’
‘Well, all I know is that gases are less soluble in hot water than in cold, but you’ll have to ask one of the physic masters if you want it explained more fully. Anyway it works very well.’
It did too. Next day I stretched my poor dead worm out on a cork board and stuck a pin through both ends. Then I picked up my shiny scalpel and made a cut carefuly down the length of it. I pulled the cut edges apart and pinned them out so that the innards were exposed. Yes, there were five hearts; how exciting!
‘What sort of blood do worms have, sir?’
‘They have the same red pigment, haemoglobin, that we have to carry oxygen, but it isn’t contained within blood cells like ours; it is just in solution in the plasma. They have lots of blood vessels in their skin, and they use their skin to absorb oxygen rather like we use our lungs. Simple but effective, eh?’
I was very proud of my dissected worm. I was going to visit mother in hospital at the weekend; she had had an operation[1] for her duodenal ulcer. I would take a dissected worm[2] like this to show her; she would be sure to be interested.
Putney
I hated the warts on my hands. They were so big and so ugly. I looked at them with horror and wondered if they were really part of my body. It was difficult to believe that they were. After all the rest of me was all right
‘Mum,’ I said. ‘Can they do anything about these warts? I’ve just got to get rid of them. They’re so ugly.’
I looked at the group of five spread across the knuckles of my right hand. Grotesque That was the only word for them.
‘They can freeze them off with carbon dioxide snow, you know.’
‘Freeze them off with carbon dioxide snow? That sounds pretty painful to me. Does it hurt?’
‘A bit, I believe, but not much. Why don’t you go and see the doctor and ask him to send you to the skin department at the hospital? They would soon sort them out for you.’
‘OK, Mum, I will.’ And I did.
It was a very painful business indeed. Not so much at the time that they did the freezing because the wart and the area of skin surrounding it became quite numb with the cold. It was when the feeling returned ten minutes later that the excruciating throb began. I looked with disbelief at the huge tense watery blisters. They were exquisitely tender. How could they have done it me? And yet, sore as it was, it was good to see the warts lifted up onto the top of the blister like so many stranded jellyfish. Surely they would go away now. Most of them did disappear at first, as the dead skin of the blister sloughed off after a few days, but there seemed to be just a hint of wart left in the middle of some of the weeping ulcers that were left behind. Sure enough many of the warts slowly but inexorably re-grew. It was such a disappointment.
My warts stayed with me until the summer of 1954 when they disappeared quite suddenly over one six week period. During this time Ivor and Trevor and Warwick and I, on vacation from college, laid gas pipes for the SE Gas Board. I repeatedly knocked them on the sides of the trench we were digging, and I think they just gave up the unequal struggle. Certainly it was less painful than carbon dioxide snow.
Epsom, Surrey
It seemed amazing that after only two more terms I would be leaving Epsom. What would the future bring, I wondered, and was there anything that I needed to accomplish before I left? Perhaps I should try to win one of the school prizes There were lots of them around and it would be fun to have a go. Why not? Although I had won a prize for Latin and Greek in the School Certificate exam, that was something I had not knowingly competed for, as I had not known that the prize existed until the letter arrived. No, it was time I did set out to win something.
I asked the headmaster’s secretary for a list of the various competitions. The next one to take place was the Mrs Major Geography Prize for the best essay on a set subject. Now I had never taken geography as a subject but this was not an essay you had to write under examination conditions, but over the course a week.
I sent my name in and in due course was notified of the subject:
Forest and marsh have proved more formidable barriers to human passage than have ocean and mountain. Discuss this statement in the light of history. Essays should be not less than 2000 words and should be completed within one week.
History, eh? I thought this meant to be a geography prize. Forest and marsh? There was always Sherwood Forest. No, that wouldn’t do. And what about Hereward the Wake? They couldn’t find him in the marshes, could they? Still that was a bit feeble. No, I could not think of any great historic journeys through forests or marshes, but mountain and ocean were different: Hannibal had crossed the Alps with his elephants, hadn’t he? And then there was the Kon-Tiki expedition that proved the Polynesians were really descended from the Incas of Peru? That was thousands of miles, and all that balsa wood!
For the next week I spent all my spare time in the library, paraphrasing bits out of dozens of different books. I might not have taken geography as a subject at school but I was certainly going to submit an essay that was longer than anybody else’s. I wrote five and a half thousand words and, despite all the plagiarism, duly won the prize, which was a book of my choice. I chose a book on anatomy and physiology so that I would feel like a real medical student even if I was still at school.
When I was given the book at the prize giving ceremony on Founder’s Day I was delighted with it: Handbook of Physiology and Biochemistry, by R.S. McDowall, Centenary edition (40th). On the front of the book was they had had the college crest embossed in gold with the motto underneath: Deo non fortuna, which we always mistranslated ‘By God, no money’. I opened it excitedly. What fascinating things would I find?
The book fell open in the middle of the chapter on respiration.
There was a square diagram in the middle of the page. The upper left part of the square was blue and the lower right was red. There was a thick black curved line separating the two colours and two dotted lines as well. Underneath it said:
Dissociation curve of haemoglobin in the actual blood at 37o and 40 mm CO2.. Blue, reduced haemoglobin; red, oxyhaemoglobin
Now I did know something already about how haemoglobin in the red cells carried oxygen but clearly there was much more to be learnt. Further on I read
The atmospheric pressure at the summit of Mt. Everest (29,000 ft) is about 250 mm and the oxygen pressure about 50 mm.
I looked at the chart again: the ‘x’ axis was labelled Oxygen Pressure in mm of Mercury and it started at 0 and went up to 100. The ‘y’ axis was labelled twice: on the left side it said Volumes of Oxygen per 100 cc of blood and on the right side Percentage saturation of Blood with Oxygen. I ran my eye up from the point where it said 50 mm Hg on the x axis and found that it crossed the thick line separating the two colours at a point corresponding to 80% saturation or 14.8 volumes of oxygen per 100 cc of blood. So that’s what would happen at the top of Everest It did not seem to be very much; no wonder that they took oxygen cylinders up the mountain with them.
I turned back a few pages. Now what was this?
The Respiratory Quality of air.-From what has been said it is evident that the air in contact with the blood is that of the alveoli.
I knew about alveoli from my biology lessons; they were the tiny air sacs at the end of the bronchioles.
From the following table its composition may be compared with that of the atmosphere and of the expired tidal air. It is to be understood, however, that these figures may vary in different circumstances, but the averages obtained from normal individuals at rest are sufficiently important in an understanding of respiration to be committed to memory.
OK then. I would commit them to memory .
Atmosphere
Expired Air
Alveolar Air
Oxygen
20.96
16.0
13 - 14
% by volume
Carbon dioxide
0.04
4.4
5 - 6
% by volume
Nitrogen
79.0
79.6
80 - 82
% by volume
Well, that was that then. I learnt the table, and I never forgot it.
Guy’s Hospital
The first patient that I clerked as a student on the wards was a lady who felt aggrieved by life; she had once been well to do, but had fallen on hard times and she resented it bitterly.
‘I should not really be here,’ she said. ‘I’m used to better things. You have no idea how upsetting it is to be on an ordinary ward.’
She said it in a voice that made it quite clear that she was the sort of lady who would normally consult a surgeon privately and not as a Health Service patient. I tried to get her to talk about her symptoms but she kept reverting to the subject that was bothering her.
‘It isn’t fair, really it isn’t. If my husband were still alive he would never had let it happen.’
Her unpleasant manner made me even more nervous on the ward than I was already and she undoubtedly has coloured my thinking about private practice to this very day.
Many things on the wards surprised me. For example, in the evening the nurses carried all the vases of flowers out of the ward.
‘Why are they doing that?’ I asked one of the second year students.
‘Oh, that’s because Florence Nightingale used to do it. Apparently she thought that it was all right to have flowers on the ward during the daylight hours as she knew that green plants absorbed carbon dioxide and gave out oxygen during photosynthesis. But at night it was the other way around. So when dusk comes, out go the flowers.’
‘But surely a few flowers can’t really make any real difference in a big ward like this, can they?’
‘No, of course not. But try telling that to the Sisters.’
‘I don’t think I will.’
‘No, I shouldn’t. Anyway it is harmless enough as traditions go.’
The following week one of the nurses tripped and sprained her ankle as she carried a large pot of chrysanthemums through the door. Perhaps it was not such a harmless tradition after all.
I was enjoying the obstetrics course immensely, though it cannot be denied that romance was a more important occupation at the time. Following the party at Ivor and Marilyn’s house in Putney (Ch.11: 1957a), and that splendid barefooted run by Isabel along the Upper Richmond Rd to catch the train back to Guy’s, Isabel and I had been out together on no less than thirty five of the next thirty six days. By which time there was a clear understanding between us that one day we would get married. I was a changed man. My casual attitude to matters of dress had disappeared. I now polished my shoes and pressed my trousers. Such is the power of love!
I found it most exhilarating to be involved with the birth of babies. I was taught how to encourage a mother to push until the babies head was almost crowned. Then to get her to pant instead of pushing while I delivered the head slowly and gently, so that there would not be any sudden changes of pressure inside the babies skull.
One day I delivered a baby boy who was pale and limp and did not breathe. I watched as the midwife first held the tiny child up by his feet so that the fluid in his mouth and throat could drain and then she slapped him on his buttocks and on the soles of his feet, trying to stimulate him to take his first breath. Nothing happened. She lay him on his back on top of a small table down and passed two fine rubber catheters over the back of his tongue, down his gullet and into his stomach. She connected one of these tubes to an oxygen cylinder so that there was a gentle flow of oxygen into the baby’s stomach; she placed the open end of the other tube so that it dipped into some water that she had in a small bowl by the baby’s side. I had heard of ‘intragastric oxygen’ but this was the first time I had seen it given. I watched the stream of little bubbles emerging beneath the level of the water preventing the pressure in the stomach from getting too high. Still nothing happened; I became fearful that the tiny boy would die. Then to my great relief the baby gave a gasp, and then another and another. He began to look pink. A moment or two later he was crying lustily in his mother’s arms.
‘That was amazing,’ I said to the midwife. ‘Can babies really absorb oxygen from their stomachs?’
‘I’m not honestly sure,’ she replied, ‘but some people think so, and it doesn’t appear to do any harm, while it might be doing some good. I have noticed, though, that babies seem only to get better after they have taken a breath. I have never seen one go pink before they have breathed even if they are given intragastric oxygen.’
‘Oh.’
‘The doctors think that it is better if you put the tube into the trachea and insufflate oxygen that way but you have to be very skilful to do that.’
Later I talked to one of the obstetric registrars about it.
‘Yes, I’m sure it is better to put the catheter into the trachea. JBB says that he always passes a catheter by touch, though I have never actually seen him do it; everyone else uses a laryngoscope. But intragastric oxygen is something that anybody can do; in Plymouth the district midwives carry two catheters and a Sparklet oxygen bulb in their delivery bags.’
It seemed strange and wonderful, and yet rather unlikely. I wondered if the midwife was right all along when she said that intragastric oxygen only worked once the baby took a breath.
Taunton, Somerset
I was perhaps getting rather overconfident. I had by now anaesthetised some twenty women for emergency Caesarean section and I was beginning to wonder if it was really necessary to put a large bore stomach tube down each of them. I hated doing this, but when I talked it over with Arthur he was adamant about it. I knew that most of the anaesthetists in the hospital made it a routine in emergency obstetric cases, but nevertheless there were one or two of them that occasionally found a reason for justifying leaving it out.
This particular Sunday morning when the phone rang at four in the morning it was Eddie.
‘Hello, John. Sorry to wake you at this unearthly hour but we need your help. We’ve got a lady here who is booked for elective section at the end of the week but she has gone into labour early. When she came in late last night I thought she would last till morning but she won’t.’
‘When did she last eat?’
‘Not since six last night. That’s ten hours ago now.’
Good, I thought, I won’t have to empty her stomach.
‘I’m on my way, Eddie. Could you give her some atropine, please?’
When I got there I mixed up some Pentothal and got the Scoline from the fridge while the midwife fetched the patient.
‘Hello, Mrs Evans, I’m just going to give you a little injection and you will soon be off to sleep.’
I chose a vein on her forearm and slipped a Gordh needle into it. I injected the Pentothal. I waited for a few moments till she became unconscious and then quickly injected the Scoline. Just as I finished doing this the lady half sat up and began to vomit copiously. There were pints and pints of the stuff. I watched with horror as it trickled down her chin and out of her nostrils. She retched again. Clearly I had not given her enough Pentothal and she was still light enough to vomit actively so she was probably still able to shut her larynx, thank heavens. I thought about the relaxant drug that was even now on its way round the circulation. When it arrived at the muscles and they twitched and lost their power to contract she would be defenceless against the vomit still in her mouth. She would not be able to keep her larynx shut and there would be nothing to stop it going down her windpipe. What should I do?
But there wasn’t time to think.
‘Hold on to her legs,’ I shouted at the midwife who was there to help me, and I tipped the top half of the patient’s body over the side of the trolley so that her head and shoulders were hanging upside down . The fluid that she had vomited drained out of her mouth and nose. I clapped the anaesthetic mask onto her face and pressed the emergency oxygen button so that the bag filled with oxygen. I squeezed the bag vigorously and, as the vomit drained downwards into the mask and the tubing which led from the anaesthetic machine, the oxygen bubbled upwards through the vomit and filled her lungs. To my relief she remained a wonderful pink colour throughout.
When the Scoline had worked and I had sucked out her mouth and throat with the sucker we lifted her back properly onto the trolley and I thrust an endotracheal tube down her trachea. The moment of crisis had passed. The operation was otherwise uneventful and mother and baby did splendidly.
It was many a year before I anaesthetised a woman in labour without first putting down a stomach tube.
I swotted for the Diploma in Anaesthetics of the Royal College of Surgeons examination largely by reading and re-reading my copy of Synopsis of Anaesthesia but I made a point of going through the three issues of Anaesthesia for the year so far. They were fascinating, though there was much that I could not understand. (For comment on the January issue see chapter 5).
The April journal began with an article on The control of consciousness which I found very difficult to follow. The next was on The prediction of carbon dioxide tension during anaesthesia by a Dr Nunn, who was research fellow at the Royal College of Surgeons and a consultant anaesthetist at the Hammersmith Hospital. Although this, too, was complicated, it was easier to understand.
It is probable that, from the earliest days, concern has been felt about the effect of anaesthetic agents upon the gases carried by the blood. In the eighteenth century ...
I looked again at the word ‘eighteenth’; what an amazing and unlikely word it was!
Beddoes noted the change of the colour of the blood: ‘I thought it might be an amusing spectacle to see the different tints of blood flowing from a wound by a leech in consequence of breathing different airs. The purple from the nitrous oxide was very evident’.
Of course, the purple blood was nothing to do with the nitrous oxide, merely the lack of oxygen, and deliberately applying a leech to create a wound that would bleed was unimaginable. What tough folk those early researchers were.
In 1847 Mr Hale Thompson of the Westminster Hospital recorded that ‘...under the full effect of ether, the arterial blood presents it usual appearance. Nor is there any reason from the inhalation to suppose that asphyxia can take place, as the usual quantity of air is admitted to the lungs’.
It was appropriate that the earliest thoughts should be directed towards the possibility of oxygen lack rather than to carbon dioxide excess - the former condition being far more dangerous than the latter...
... the alveolar carbon dioxide concentration is the result of the balance between production and elimination (rather like the blood urea)...
And a bit like my bank balance! One day I hoped that I would be producing money faster than I was spending it. Only last week I had had a letter from the bank manager pointing out that each month I was spending about £10 more than my pay cheque. While he was not particularly worried by this he thought that I should bear in mind that one day I would need to reverse the trend .
Further on there was a paper about a new drug for premedicating children. It was called Trimeprazine tartrate, and had antihistaminic, antiemetic and sedative properties. It sounded marvellous. I would have to try it out.
I picked up the July issue and opened randomly. Here was a paper on The economics of anaesthesia. Apparently in the Southampton group of hospitals the cost of an anaesthetic was not very much:
...by and large, I think these figures show a commendable economic modesty on the part of our specialty. The skill required, the responsibility involved, the benefit to the surgeon and the patient, let alone the pleasure derived by the anaesthetist in the giving of a well-administered anaesthetic, are remarkably cheap at the average price of £3 13s 9d.
A few pages on there was a nice little article reporting that halothane and chloroform did not in themselves alter the oxygen dissociation curve of blood. As this paper only occupied half a page of text it was a splendid model of brevity, but as it was only reporting a negative result I supposed that was fair enough.
Now I turned to the front pages of the journal; here there was an article from Newcastle that immediately caught my interest - On the efficiency of intragastric oxygen. It started:
The introduction of oxygen into the stomach and intestines of neonates is widely used in Britain in the treatment of anoxia.
Well, not as widely as it had been. I knew many people nowadays thought that it was a poor substitute for ventilating the lungs, but where the skill necessary for this was not available, no doubt it was still in vogue.
The paper went on to describe experiments on newborn kittens which proved that oxygen transfer across the gut could contribute not more than 7% of the minimum needed for bare cardiovascular survival - I presume they meant to keep the heart beating. So here was real evidence that intragastric oxygen could not work But then I never had really believed it would. I had once wondered whether feeding oxygen up the ureter might be better; after all the kidney had a huge blood flow through it and the surface area of the millions of glomeruli was enormous; of course that was altogether too fanciful.
‘What are you reading about, John?’ asked Isabel.
‘Oh, about intragastric oxygen.’
‘Never mind about that, dear. Supper is ready. Come and have some intragastric bacon and eggs; it will do you far more good.’
‘That’s certainly true[1],’ I replied.
Catterick, Yorkshire
‘Have you seen the BJA?’ asked Jeff.
‘No, I haven’t. Why?’
‘There’s a symposium on Vomiting in Anaesthesia. It looks really interesting. For example, did you know that in the early part of this century they used to try to prevent postoperative vomiting by squeezing the patient’s nostrils, raising the head of the bed twelve inches, using perfumed gauze towards the end of the operation and putting a mixture of potassium bromide, aspirin and glucose into the rectum?’
‘Sounds kinky to me.’
‘No, seriously, it looks like a good selection of papers. One of them says that there is less vomiting these days because we are using less ether and cyclo and smaller doses of opiates, and another says that perphenazine and haloperidol the best anti-emetics.’
‘What about cyclizine? I have always thought cyclizine was the best. After all, it’s what they gave the troops when they crossed the channel on D-day[1].’
‘I’m not sure what it says about cyclizine; I only skipped through it quickly. You’ll have to read it for yourself. But there is a good article on the induction of anaesthesia by Dr. Inkster from Newcastle. He describes how they deal with the problem of the full stomach at the Royal Victoria. It is pretty amazing.’
‘Why what do they do?’
‘Well, first they don’t use thiopentone or relaxants so that the diaphragm does not lose its tone suddenly on induction and they don’t get gastric juices regurgitating into the pharynx. They use a gas induction and they turn the carbon dioxide up really high to make the patient hyperventilate. That way he can’t stop taking in the ether they are giving him, even though it is so irritant, but more important he cannot actively vomit, because you just cannot vomit and overbreathe at the same time. I’ve tried it and they are right. You just cannot do both together; the reflexes are mutually exclusive. Think about it for a moment.’
I thought about it. Yes, of course, to overbreathe you had to open your glottis; to vomit you had to close it. You could not do both things at once.
‘That’s sounds a good idea. We used to give CO2 in Taunton to hurry up an ether induction but it wasn’t to deal with the full stomach. Anyway, when we used it for Caesarean sections we just stayed with the facemask, or at least Dr Jones did. I’ll give a whirl sometime.’
‘Inkster says that they have been using this method for the last fourteen years and that during this time there has been no instance of a fatality from inhalation of vomitus during induction of anaesthesia. It certainly sounds OK.’
Later in the day I read the article carefully, and that night when I was presented with an emergency case who had a full stomach I used the technique exactly as Dr Inkster had described:
The facemask is gently but rapidly lowered on to the patient’s face, nitrous oxide, 10 l./min flowing from the machine. After the first ten breaths, the rotameters are adjusted so that nitrous oxide 8 l./min, carbon dioxide 2l./min and oxygen 2 l./min are delivered. A further ten breaths of this mixture are allowed, and hyperventilation commences. Consciousness is lost late in the first phase or early in this, second, phase. During the third phase, i.e. the succeeding ten breaths, volatile agents are introduced. The nitrous oxide is reduced to 7 l./min and the carbon dioxide flow is reduced to 1 l./min. Ether vapour is introduced in stages so that, at the end of stage three, the tap of the vaporiser is fully open. During the fourth and last phase of the induction the oxygen flow is increased to 3 l./min and the carbon dioxide is turned off or reduced to 500 ml/min, depending on the extent to which the patient is hyperventilating. The ether concentration is further increased in stages until the plunger is fully depressed below the surface of the ether. This takes ten or fifteen breaths and, at the end of this time, the conditions required for intubation will have been achieved.
After the forty-fifth breath I lifted the facemask, slid the laryngoscope into the patient’s mouth and onwards down his throat to expose his larynx. Then I thrust the endotracheal tube between his vocal cords. It worked like magic.
Despite the brilliant success in a series of one, I thought that probably I would not go over to the technique routinely as you still had to convince the patient that a gas induction was best and most of them did prefer something intravenously. Anyway, now that I was giving patients with full stomachs oxygen for a few moments before putting them off to sleep and using cricoid pressure as well, things seemed much better than they had been than when I was dealing with all those emergencies in Taunton.
It was always interesting to be ‘with J.C-B’, which is how the duty roster described it when you were deployed to help the senior lecturer[1] with one of his theatre lists. He was an remarkable man with an amazing way of getting to the nub of a problem in just a few brief moments and then letting the conversation wander off in a different direction, sometimes more than one direction at once. I recognised only too well the symptoms of a grasshopper mind, for I knew that I had one myself, though, of course, I lacked J.C-B’s incisive and penetrating mind.
One day I asked him to tell him more about his experiments on pain.
‘P-p-pain is a fascinating subject,’ he said. ‘A-aristotle called it ‘an agony of the soul’, while Sherrington said it w-was ‘the psychic adjunct to an imperative protective reflex’. I prefer the Aristotle myself. T-tell me, when you hit your thumb with a hammer what do you do? Do you hold your breath or do you h-hy-perventilate?’
I thought about it for a moment. I tried to remember the last time I had hit myself as I knocked a nail into the wall.
‘Oh, I take a deep breath in, hold it for a moment or two, while I dance on one foot shaking my hand, and then if the pain doesn’t go away I take long deep breaths which I guess mean that I do overventilate.’
‘Yes, acute p-p-pain certainly makes one increase one’s alveolar ventilation. The people in Liverpool think that you can get useful analgesia if you hyperventilate your patients during surgery, but I think this may be the result of less oxygen getting to the brain because the arteries are constricted by the reduced carbon dioxide levels. You’ve seen our spring balance, haven’t you?’
He was referring to the modified kitchen scales that I had seen him use to measure pain thresholds on volunteers. The pan of the balance had been replaced by a round-headed screw, which he pressed against the subject’s shin until the subject said he felt pain or responded by withdrawal of his leg. When this happened the pain threshold was read on the scale of the balance.
‘Yes. It looks very uncomfortable to me.’
‘Oh, it’s not really. It just leaves a few bruises that hardly bother you at all. You have to use a different spot on the shin for every reading, of course. Anyway we looked at the effect of overbreathing in volunteers and we showed that it produced some degree of general analgesia in five out of six subjects. We also found that breathing oxygen returned the pain threshold nearly to normal and that taking a breath of amyl nitrite put it right back to normal. So I don’t think we should hyperventilate our patients like they do in Liverpool; the vasoconstriction may be causing cerebral hypoxia.’
He broke off to talk to the patient as he always did during the operation.
‘Everything is going very well, Mrs Smith. Are you comfortable?’
Though the patient had a tube down her windpipe, was being ventilated by a machine with 75% nitrous oxide and appeared totally oblivious to the operation that was going on, she nodded in response to the question.
‘That’s good,’ said J C-B.
‘Of course,’ he said to me, ‘we do not actually know what this lady’s CO2 is doing. Even now we are probably erring on the side of overventilation, though I really don’t think a little respiratory acidosis would do her any harm. It might even be good for her - she would have a nice bounding pulse and a good peripheral circulation, and the O2 dissociation curve would be shifted to the right so that oxygen would be released easier at the tissues, though the operation site would certainly be more bloody.’
‘It is a pity that we cannot measure the CO2.’
‘We do during the heart cases, of course, as the information we get is certainly worth the trouble of setting up the infrared analyser. I’ve no doubt that one day the technology will be simpler and more reliable and then we will use it much more frequently, if not all the time. Maybe we don’t measure enough things during anaesthesia at present but that’s largely because we are not certain what it is that is best to measure. I’m quite sure that an experienced anaesthetist watching the patient closely is better than a lot of complicated machinery giving you information that you might not really want. Of course, if you are not going to watch the patient then you will need machines to do it for you, but we need some that something better than those available to-day.’
‘Yes, it is a pity that the CO2 analyser is so big and clumsy.
‘And it also takes two hours to warm up and needs two cylinders for calibration. I did once make a simple analyser from bits lying around the department, using the Wheatstone bridge principle.’
‘How do you mean exactly?’
‘Well, it was like a pneumatic version of the Wheatstone bridge. Instead of electrical wires I used tubing and made up a divided circuit with an U-tube manometer across the bridge in place of the galvanometer. I used a container with sodalime as one of the resistances, and drip tubing controllers for the others. I put a sucker at one end and sampled expired air at the other. It was a bit Heath Robinson but it worked all right. You could see the meniscus in the manometer swinging with the different phases of respiration.’
‘That’s amazing I must try that one day.’
‘It’s rather important that the flow produced by the suction is kept constant; if it isn’t then you can get a swing that is not due to changes in CO2 at all. One way of doing that would be to use a ‘critical orifice’.’
‘What’s a critical orifice?’ I asked.
‘Oh, if you have an orifice below a critical size for a particular gas, and suction above a critical value then the flow through the orifice is constant even if the suction does vary. So you could have something simpler than a Wheatstone bridge. Just a tube which samples at one end, has a CO2 absorber in the middle with a manometer across it, and a critical orifice at the far end, and some suction, and the manometer movement will tell you the concentration of CO2 in the sample at any moment.’
All the time he was talking J.C-B was watching the patient closely and every five minutes or so he took the blood pressure. We were monitoring her heart with an ECG that J.C-B had made himself; it did not have an oscilloscope that you could look at, but only a galvanometer needle that swung from side to side. With practice and the eye of faith you could see the P waves and the QRS complexes, and recognise extrasystoles, though you could not spot S-T depression or bundle branch block, of course.
At the end of the operation we reversed the relaxant with 5mg of neostigmine.
‘Because we have not given her any opiates during the operation she will start breathing straight away even if we have lowered the CO2 a bit.’
He turned the nitrous oxide off.
‘Your operation is all over, Mrs Smith. You have done very well. I am just going to take that tube out of your mouth. There, that’s it, open your mouth widely while I suck some of that spittle away. That’s very good. You have done well.’
He turned to me.
‘It’s very important to talk to the patient at this stage. If she wakes up with a tube still in place and someone is putting a bandage onto her tummy, how is she to know that the operation is over unless you tell her? I think most complaints of ‘awareness’ during surgery occur because people don’t talk to the patient, particularly once the nitrous oxide is turned off.’
He turned back to the patient who was by now wide-awake. ‘Are you comfortable, Mrs Smith?’
‘Yes, thank you,’ she replied, as she was lifted onto the trolley and wheeled out of the theatre. She had very little analgesia on board, just the 50mg of Pethidine that she had had as a premed, and I knew that within ten minutes she would be asking urgently for something to help her pain.
The new Intensive Care Unit at the Royal Infirmary was open at last, due largely to Peter’s unremitting persistence and determination against all reactionary opinion, which was to be found in the most surprising of places. For example, the Professor of Medicine had opposed the unit all along, even saying publicly that no patient of his would ever be admitted to the Intensive Care Ward, or Expensive Scare Ward, or whatever it was. It was somewhat ironic therefore that the very first patient that was brought to the unit was one of his.
The ward was equipped with brand new Cape ventilators, which were splendid machines, certainly much more robust and powerful than the Cyclators, though unfortunately the Capes could not be used for triggered ventilation. Patients who needed help with their breathing were given large doses of an opiate, often this was Phenoperidine, and then were deliberately hyperventilated to reduce their respiratory drive even further.
Two of us, both registrars, another John, a good friend, and myself, manned the unit between us for a month, twenty-four hours on and twenty-four off. We learnt how to measure the patient’s carbon dioxide levels by using the instrument that Dr Campbell of the Middlesex Hospital had developed. He had started from the classical Haldane apparatus, which was horribly complicated and scientific, and had simplified it till he arrived at something which was cheap, portable, speedy and easily serviced, yet was still accurate enough for clinical purposes.
First we took a two litre rubber bag with a litre and a half of oxygen in it and then we made the patient breathe in and out of this bag for about ninety seconds, so that it began to accumulate carbon dioxide. After a two minute rest we repeated this rebreathing in and out of the bag, but this time only for five breaths, or fifteen seconds, whichever was shorter. We repeated this again after another two minutes. As a result, the contents of the bag became equilibrated with the patient’s mixed venous blood. It was amazing really; you ended up with some gas in a bag whose carbon dioxide tension was the same as that in the patient and you cold take it off to the small laboratory attached to the ward and measure it with the Campbell apparatus. True this was rather fiddly, despite Dr Campbell’s efforts, but it was definitely something we could cope with and we came to rely on it in the management of patients on the new unit.
One fine autumn morning my copy of Anaesthesia fell onto the doormat. I picked it up and browsed through the pages.
‘Look at this, Isabel. There’s a paper[1] here by Bryan, you remember, the fellow who followed me as SHO at Taunton. It sounds interesting: Some factors influencing postoperative hypoxaemia. It is about work he did while at Cambridge, but I see that he is now in Pennsylvania; that sounds fun.’
Later in the day I found time to read it properly. It was clearly a very important paper. Bryan and his co-author Dr Millar had taken several groups of patients and studied what had happened to the oxygen and carbon dioxide levels in the blood before, during and after their operations.
They showed clearly that there was a bigger drop in oxygenation after surgery when the patient was old, had pre-operative lung disease, was given a narcotic premed, underwent a long operation, was ventilated by a machine or had an abdominal incision.
If you were young with normal lungs, had a short operation, which was not an abdominal one, during which you breathed for yourself, then you would be OK once you had got rid of the nitrous oxide you had absorbed, which would take about five or ten minutes.
They also pointed out that the old people who had the biggest and most prolonged fall in their oxygenation were also the very people who were least able to compensate for it by increasing their respiration and cardiac output.
Well done, Bryan! A thoroughly useful paper which over the years I have repeatedly quoted when teaching junior anaesthetists. I meant to write to him to congratulate him, but I never got around to it.
The surgeon was an unusual man. He had what I later came to recognise as the syndrome of ‘low peripheral movement’. When he talked, as he occasionally did, he did not wave his arms around, or shift from one foot to the other, or scratch his backside, or run his fingers through his hair, or do other things that could be classed as normal, though unnecessary, fidgeting. He stood very still. His immobility gave him an uncanny and rather disconcerting presence. As he was also a most unlikeable individual, appearing to lack warmth and kindliness towards the human race in general and his colleagues in particular, it was not surprising that he had a formidable reputation. Peter used to say to new registrars
‘If he asks you anything just say ‘100’; it will do for the temperature, the pulse or the blood pressure.’
This was not, of course, always true, for these were the days of ‘profound hypothermia’, or the ‘big freeze’ as it was affectionately called. I had never seen anything like it. One day we were operating to repair a ‘hole in the heart’, properly called an atrial septal defect. The hole, which was situated in the wall between the two smaller of the heart chambers, allowed blood from the stronger left side of the heart to leak back into the weaker right side of the heart and so flood the lungs. The surgical team had first carefully split the sternum in half from top to bottom. Then they had replaced both sides of the young patient’s heart with pumps and used his own lungs to oxygenate the blood in the normal way. This meant that they had been able to cool him down by pumping his blood through a heat exchanger and not have to worry about the circulation when the heart ‘arrested’ as the temperature fell to unphysiological levels. When it had fallen to 8oC they had stopped the pumps, and the ventilator as well, as the boy was cold enough to survive without any blood flowing. Now they could operate on the heart as easily as though it had just come out of a fridge in a butcher’s shop. It was truly staggering.
I put my hand out and rested it on the small boy’s forehead. It was as icy cold as though he had been in the mortuary for a week, and yet I knew that if all went well he would be awake and talking before the afternoon was over. It was truly amazing.
Geoffrey explained about the ventilation and the problems they had had during the first few cases.
‘If we use a fresh gas flow of 6 litres per minute we do not need to turn on the carbon dioxide absorber while the temperature is normal. Now that we can measure the CO2 we have found that six litres a minute is quite adequate. As we cool the blood we actually have to begin adding carbon dioxide to the inspired gases in order to keep the end tidal level at about 5%. This is because carbon dioxide is so much more soluble in cold blood than it is in warm blood.’
It was fascinating to watch; by the time the patient was cold enough to tolerate circulatory and respiratory arrest we were ventilating him with 10% CO2. This would have been disastrous for him if his temperature had been normal.
‘How many cases of these cases have you done now?’
‘Oh, about fifty I should think[1], though we had terrible problems at first as we did not realise how much carbon dioxide we needed to add to the inspired gases. Now it is all rather routine.’
Rather routine, indeed! I touched the child’s forehead once more to convince myself that I was not imagining it. But, no, I was not.
‘Of course, it will all have to come out again when we warm him up after the hole is repaired, and in addition if he has a metabloic acidosis, we may have to give him some sodium bicarbonate as well; that also has a ‘fizz effect’.’
By this he meant it also gave off carbon dioxide, like a bottle of lemonade when the top is unscrewed.
The operation went well. Later, when he was back in the cardiac unit where he would be nursed for the next week or so, I asked him how he was.
‘All right, thank you,’ he said politely from behind the oxygen mask. ‘Though it does hurt rather a lot.’
I injected some more morphine directly into a vein in his arm. Soon he was sleeping.
Working with the cardiac surgeons was certainly a busy job. Monday was not too bad; I could rely on getting home for the evening and the night. From then on it was different: I regularly used to leave home at a quarter to eight on a Tuesday morning and not get home again until late on Friday evening, and then only for an hour or two before going back to check that everything was all right. Things were so bad that Tim said to me one day
‘Hello, Daddy. It is nice to see you. When do you have to go back to your home at the hospital?’
On another occasion the senior consultant in the anaesthetic department rang home:
‘Is John there?’ he asked.
‘John does not live here any more,’ Isabel snapped back. ‘Try Bristol 22041’, and she put the phone down.
I was despatched home within the hour.
When I arrived home I said in a deliberately reproachful voice
‘Isabel, I could hear you shouting at the children from the bus stop.’
‘You don’t want to worry when you can hear me shouting, John,’ she replied. ‘It’s when you can’t hear me that you need to run’
Poor lass, it might be hard work for me at the hospital but I guess it was even harder looking after three children under six with no husband to support you.
One day we had a 44-year old lady for closed mitral valvotomy. She had been breathless for eight years and it was getting worse.
The operation went well enough but at the end of it she remained drowsy with intense vasoconstriction and cold blue feet and hands. Her blood pressure was 90/60, her pulse rate 56 per minute, and her central venous pressure +10 cm. We left her endotracheal tube in place for an hour or so, but then, as she seemed improved, we took it out. We left her breathing for herself with an oxygen mask.
She did well for the next six hours but when I went back later to the unit to see if she was all right, it was clear to me that she was working harder at her breathing than she had been earlier. I listened with a stethoscope to the back of her chest and found that her lungs were now rather wet. I looked at her charts: her temperature had risen to 101oF and her respiratory rate had gone up in the last half hour from 22 per minute to 28 per minute, though her pulse rate and blood pressure were unchanged.
Now several days previously it had occurred to me that I might be able to assess a patient’s oxygenation by looking with an ophthalmoscope at his or her retinal vessels, which are the blood vessels at the back of the eye. Here you would be able to see, under a standard light source, the colour of the blood in both the arteries and the veins; this might be very useful and might even allow you to deduce how well the heart was pumping blood around the body. This seemed an ideal occasion to put the notion to the test.
I got an ophthalmoscope from the equipment trolley.
‘I’m just going to look in your eye for a moment, Mrs Morris. Look at the picture on the wall over there and try to keep your eye still. Good.’
I could see the retina at the back of her eye quite clearly. The blood in the arteries was certainly not as brightly red as it should have been, and the blood in the veins was very dark blue indeed. Oh, I thought, her arterial blood is less than optimally oxygenated, and her cardiac output is reduced.
‘I think we will need to ventilate her again,’ I said to the nurse. ‘She has started to make heavy weather of things. I’ll just take some blood samples while you get the Cape ventilator ready.’
First I took a sample from the artery at her wrist. Often we already had a cannula in an artery in patients that had heart surgery, so that we could bounce the pressure inside it against a U-tube of liquid mercury, but on this occasion I had to pierce the artery with a needle to get the sample. Then I took a syringeful of blood from the long cannula that ran from the bend of her elbow up a vein to reach one of the large central veins. So now I had both arterial blood and central venous blood. I nipped upstairs. The machine was called a ‘reflection oximeter’. You had to calibrate it with fully oxygenated blood from the patient and also with fully deoxygenated blood; you converted these to cyanhaemoglobin, put them in a special cuvette and shone red light at the surface; the amount of light absorbed or reflected depended on the ratio of red pigment, oxyhaemoglobin, to the blue pigment, reduced haemoglobin. It was quite a palaver As one of the agents used was potassiun cyanide you had to be careful not to get it onto your fingers.
It took me some time before I got any reproducible results from the oximeter. Then I had to draw a calibration graph and enter the values from my samples; the arterial oxygen saturation came out at 80% instead of the normal 97%, and the venous at 30%, instead of the normal 75%. I was surprised as she had not looked as blue as that, though I had noted how dark her retinal arteries were. It must have been the lighting in the ward that had stopped her looking blue; the colour of a patient’s lips and skin is very dependent on the spectrum of the available lighting. No wonder it was always said that low oxygen was something you could not always detect clinically. It had been better to look at her retinae, because the light from the bulb had not distorted the colour as much as the light in the ward.
I hurried back to the cardiac unit. Mrs Morris’s breathing was worse if anything, so I explained to her what I was going to do. I gave her a small dose of thiopentone and a large dose of Phenoperidine to send her asleep, and some Scoline, which relaxed her muscles. Then I popped a tube down her windpipe and connected her up to the ventilator.
‘We will also give her some Lasix to dry out her lungs,’ I said. ‘The positive pressure will do that anyway, and by putting her on the ventilator we are resting her heart as it does not have to supply so much oxygen to her muscles to cope with the work of breathing. I’m sure she will be all right.’ I picked up the ophthalmoscope and looked into her eyes again; now the arteries were a wonderful bright red and the veins were much less blue than they had been.
‘That’s better,’ I said. ‘Her blood looks fully saturated, and the difference between the arteries and the veins is certainly less marked than it was, so her heart must be working better too.’
I took new blood samples and repeated the measurements. I was delighted when that my predictions were proved to be correct: the arterial blood was now 100% saturated and the central venous blood was 60%.
After that I regularly used an ophthalmoscope in the assessment of patients who might have low oxygen in their blood.
Chicago, USA
‘What have you got in that bag?’ the Customs Officer asked Isabel.
‘It’s full of dirty nappies, but you are welcome to look if you like.’
‘Why, no, Ma’am. That won’t be necessary. Have a good day.’
We were only in Chicago for an hour and then we were on our way again. Because I was such a heavy smoker and I knew that Denver was a mile high in the sky I half expected to feel short of breath when we got there. But I did not.
Bob and Mildred met us, and Rob and Shirley were there as well. Between them they made us feel very welcome and they ferried us to our apartment in the block of flats in Cherry St.
Bob said ‘Now you get yourselves settled in and you, John, can come along to the hospital about 11 o’clock in the morning to meet everybody.
‘’Are you sure? I could come earlier if you want.’
‘No, 11 o’clock will be fine.’
We were very tired and we fell asleep as soon as our heads touched the pillows. As our inner clocks were still six hours ahead of Denver time it was no surprise when we woke at five o’clock.
‘Does it feel as though you are a mile up in the sky?’ I asked Isabel.
‘No. It feels just like sea level to me. Should I feel different?’
‘Not really, unless you took some vigorous exercise; then you would probably get out of breath very quickly. You are only breathing about 83% of the oxygen that you are used to at home, you know.’
‘That seems strange. Are you sure that it’s OK?’
‘Oh, yes. We’ll soon raise our haemoglobin levels, reset our respiratory centres and grow more heart muscle.’
‘It doesn’t sound very nice to me. Shall we get up?’
By six thirty we were out walking. We did not know at that time that no one in Denver ever walked anywhere.
By nine o’clock Timothy was enrolled and installed at Palmer School.
By ten o’clock Isabel had the nappies washed and on the line. We discovered later that none of our neighbours in the apartment block had seen washable nappies before (nor a male infant that had not been circumcised).
By eleven o’clock I was at the hospital where I met the other members of the department and learnt about the anaesthetics and the equipment that they used. Everything was so different: there were no cylinders of carbon dioxide on the anaesthetic machines and the oxygen cylinders were painted green. It was all very fascinating.
At the weekend we went with Rob and Shirley and their two children up to Echo Lake, which is at 10,000ft. This was well above snow level but was still below tree line. The sun shone brilliantly and the whole experience was utterly exhilarating. I did notice that I was slightly short of breath but nobody else seemed to be bothered at all.
At work on Monday I asked Dave what the barometric pressure was at 10,000ft.
‘Oh, about 520mm Hg,’ he replied. ‘So you were probably breathing about 14 or 15% of the oxygen at sea level. Still you have been in Denver for nearly a week now so you will already be partly acclimatised to 5000ft. If you felt breathless it was probably due to all those cigarettes that you smoke. I guess your blood must contain nothing but carboxyhaemoglobin.’
‘I expect you are right. I really must try to smoke less.’
A few days later it became clear that I needed a bank. I resisted the temptation to go to Wells Fargo, even though they had a stagecoach on their cheques, as they were awkward to get to. I went instead to the nearest and most convenient, who were giving away stainless steel cutlery to new clients. I arranged to borrow some money to buy a car and to help us survive till payday, which came around twice a month, on the 8th and the 22nd. In effect you were paid a week in arrears for the first week and a week in advance for the second. It seemed a splendid arrangement.
I bought a magnificent Dodge Coronet saloon, with power brakes and power steering, which had 120,000 miles on the clock. I paid the equivalent of £90 pounds for it, and I reckoned that I had got myself a bargain.
We had many happy weekends picnicking in the mountains but it was springtime before we got around to motoring to The Rocky Mountain National Park itself, some 40 miles away, where we climbed up Trail Ridge Road; this reaches 12,100ft and is the highest continuous vehicle-carrying highway in the USA. We stopped at the top and admired the splendid snow-covered peaks of Never Summer Range.
When we got out of the car I felt really strange. I had a whoozy feeling in my head, a slight buzzing in my ears, and the world seemed distant and unreal. It was most unpleasant. When I mentioned it to Isabel she told me not to be so silly, it was the same for everybody, though in fact nobody else complained at all.
I began to think that I was imagining my problems, but when it was time to leave I found that the car too was suffering from lack of oxygen and I had the most terrible trouble getting the engine to fire.
‘We must go to the top of Pike’s Peak too before we go back to Bristol,’ Isabel said. ‘The road there goes right to the top, though of course you can only turn around and come back the way you set out. It’s not like this road which actually leads somewhere the other end.’
So later in the year we did motor to the top of Pike’s Peak, the splendid 14,000ft mountain that towers over the town of Colorado Springs some 60 miles south of Denver. Only the Americans, I thought, would build such a splendid road to the top of a mountain just so that people could see the view.
We were by now, of course, fully acclimatised to a height of 5000ft, and were intrepid lower-slopes-of-the-Rockies people, often visiting Buffalo Bill’s grave and Central City, but 14,000ft was a different matter.
Three quarters of the way up the engine of the car started to pink and I wondered if it would make it to the top, but get there it did. Remembering how difficult it had been to start the engine on Trail Ridge Road I took care to park it facing slightly downhill.
I was certainly light-headed when I got out of the car and I stood quite still, stunned by the thinness of the air and fabulous panorama of the Rockies. It was a sight never to be forgotten, even if it did mean that you had to breathe the equivalent of only 12% oxygen at sea level.
Bristol
Now that the University, rather than the NHS, was my paymaster I decided it was time to see if I could measure the oxygen saturation in retinal vessels; to date I had just looked at them with an ophthalmoscope and guessed what was happening.
So I went up the hill to the University Physics Dept and discussed the idea with Dr Gibbs, the Senior Lecturer. To my surprise he was interested and encouraging; he suggested that he got a couple of undergraduates to set up a project and see what came of it.
A few days later he introduced me to Geoffery and Susan. I told them what I was trying to do, and how exciting I thought it was. The two youngsters entered into it with great enthusiasm.
With David Gibbs guidance they built a magnificent apparatus. It consisted of a white light tungsten light source positioned at one end of a hollow black cylinder with a lens at the other end. There were some screens, a red filter, a half-silvered plate glass, and a mirror mounted on a motor so that it rotated in a circle of 19cm radius. We put. With this set up they were able to pass beams of red light over glass capillary tubes filled either with my blood or white paint in an open-topped tank filled with glycerol the capillary tubes and measure the light that was reflected with a photocell connected to an oscilloscope. This could be photographed with a Polaroid land camera We prepared samples of blood of known saturation (or so we thought at the time) by mixing fully oxygenated blood with blood that had been fully deoxygenated by bubbling with 95% nitrogen - 5% carbon dioxide.
Geoff and Susan’s experiments demonstrated that the amount of light reflected from a capillary tube filled with blood was dependent on both the haemoglobin concentration and the oxygen saturation. When I read their project reports I was impressed by the thought and effort they had put into them. I was left wondering just how practical it would really be when applied to the human retina, whose vessels were about only one tenth the diameter of the glass tubes we had used. Also I started to worry about whether the light would have to be so bright that it would damage a patient’s eye.
I let it rest for a few weeks and then I made time to ferret through the main medical school library looking for anything that could persuade me to continue with the idea, or else abandon it. In the Journal of the Optical Society I came across a reference to an eye tracker that seemed likely to be useful, as it was designed to study the vessels at the back of the eye, though not the blood inside them. I wrote to the author, Tom Cornsweet (what a splendid name) at the Stanford Research Institute.
In his reply he told me that the current version of his eyetracker had been modified.
We put a photomultiplier where the zenon flash tube used to be, and in the plane where the film used to be, we have installed a little optical system that causes a tiny bright spot to travel a circular path 5o in diameter in the optic disk...
I noted the American spellings with interest; somehow zenon and disk did seem more sensible than xenon and disc.
... as the spot crosses the blood vessels in the optic disk, the amount of light reflected back out of the eye and into the photomultiplier is modulated... special purpose computer... we are moving the spot very fast (500 rotations a second)... one could make the sort of measurements that you are interested in...
The letter was full of casual scientific detail that made me nervous. I was clearly a babe in arms compared to this lot
In general, from what we have done here, I would guess that one could construct a device that would give a fairly accurate colorimetric measurement in vivo, but I would also guess that it would be a fairly expensive instrument and would take quite a bit of development work. (But work that sounds a lot of fun to undertake.)
The mention of fun reminded me of what J.C-B had always said about research: ‘if it’s fun then carry on with it, but if it ever stops being fun give it up and do something else’.
... another project... very high resolution photographs of the retina... so that the capillaries are clearly visible... a specially constructed fundus camera with some extra gimmicks in it, such as automsatic focussing, the pictture being recorded by a television system and manipulated electronically to overcome the aberrations of the eye... we will certainly be obtaining data on the reflectances of the retinal vessels... probably take four or five years...
Four or five years! That was an awful long time span for someone with my impatient personality, and although I was very flattered that my humble letter had produced such a full response, I was overawed by the science of it. Taking blood samples from peripheral arteries and central veins might have to do, after all.
I did present some of my ideas and our results to the Anaesthetic Research Society when it came to Bristol, but I did not offer a summary for publication as I felt altogether too diffident about it. Still it had been great fun!
Ronnie was such a quiet and gentle fellow - except for those times when he thought that Graham was being unnecessarily obstructive. Then his eyes would flash and his face become thunderous.
'I'll swing for him one day' he would mutter. 'I think he's the university's secret weapon to make sure that no research is actually completed.'
This was, of course, a thoroughly unreasonable comment; Graham could be a most useful and helpful fellow. I am not sure how it came about, but it fell to me to act as go-between and peacemaker between the two of them. I had always thought that I might have been a diplomat, and here was my chance to prove it. Somehow or other I managed to calm Ronnie down and enlist some help for him from Graham.
Ronnie was a true scientist - at least in comparison to the rest of us. He was a deeply thoughtful man, who was totally committed to his researches. His planning and execution of projects was meticulous; no detail was too small for him not to worry over till every aspect of it was sorted, physically at least; my role was to sort out the personality clashes.
So it was that I became loosely involved with Ronnie's project on the infrared CO2 analyser. We wanted to know if it could be made more accurate. It was certainly good enough for clinical decisions to be made on the strength of it, but respiratory research workers could do with something better than +/- 0.1%.
Ronnie was already an expert on the Lloyd-Haldane apparatus, which was the classical method of measuring carbon dioxide in gas mixtures, as he had used it while working in Oxford some years earlier. He now set out to become the world's expert on it rather than merely the local expert. Since the methodology was finicky beyond belief it was a Herculean task, though in due course he did achieve his gaol.
In the meantime we set about dismantling the infrared analyser and looking at the effect of temperature changes on its performance. We put the detector head in a plastic bag and dropped it into a thermostatically controlled waterbath, so that we were able to keep its temperature constant or to change it, as we wanted. The temperature of the amplifier, which was still inside the casing of the machine, was the same as that of the room; if we wanted to keep it constant then we had to keep the temperature of the room constant. It was quite a palaver trying to achieve this in a draughty ground floor room of an old Victorian house at the top of St Michael's Hill which the University had put at the disposal of the anaesthetic department.
Ronnie was in his element: there were badly fitting window frames and doors to be sealed and electric fires to be turned on at critical moments so that the temperature did not fall overnight. We found that a change in temperature of either the detector head or the amplifier caused readings to drift considerably. When we reassembled the analyser we found that after a rise in room temperature of 5o C the amplifier stabilised at the new temperature within 2 hours, but the sample cell was still rising after 5 hours.
We looked too at the effects of changes in pressure within the sample cell and the effect of changes in barometric pressure. For help with this Ronnie phoned the Bristol Meteorological Station at Filton and got information about the degree of change in barometric pressure between 9am and 12 noon for every day of the year 1969. On one day in January the swing over these three hours was greater than 5 millibars and on one day in December it was greater than 4 millibars. Despite this, on 85% of days the swing was sufficiently small that the error in the measurement of CO2 due to barometric pressure change was +/- 0.01% or less.
It was certainly very fascinating, and good fun too, but it was always Ronnie's baby not mine. I had realised from the start that I was not a 'real scientist' and never would be. Still it was fun to see my name on the paper [1] when it was published, even though I had played only a minor part in its production.
I looked at the blood gas results. The arterial oxygen tension was down again. I wondered if it would be best to raise the end expiratory pressure or to increase the inspired oxygen concentration yet again. Probably it did not really matter which I did as long as I did one or the other. We must keep the amount of oxygen in the blood at a satisfactory level whichever way we managed it. I decided to increase the PEEP.
Later in the day the surgeon and I spoke to the patient’s wife.
‘When your husband comes off the ventilator he will be much better.’
I sighed. Would the surgeons never get it in perspective? You would think we kept the patient on the machine just for fun. Could they really not understand that if we took the patient off the ventilator he would die? I leant forward and said slowly and clearly so that there should be no chance of misunderstanding
‘What Mr Manners means, Mrs Smith, is that when your husband is much better, he will come off the ventilator.’
It was such a simple difference of emphasis, and yet so fundamental. (Years later it may be hard to appreciate just how blinkered people were in the seventies.)
I was no sooner back in the lab than the phone rang. Sheila answered it.
‘Department of Anaesthetics. Oh, Hello. Yes, he is here. I’ll pass you over to him.’
She mouthed ‘it’s J C-B’ as she handed the phone across.
‘J-John,’ said the professor, ‘we have got the H-Henry Hill Hickman Club coming to visit us next month. That’s a group of anaesthetists from Chester who have formed themselves into a travelling club. They are coming to Bristol for a couple of days and I wondered if you could entertain them at Southmead for an afternoon?’
‘Yes, certainly. I’ll tell them about the research we are doing here if you like and perhaps get Peter to talk to them about the care of low birth weight babies and possibly get Barry to talk about kidney transplantation. How would that do?’
‘Oh, that would be sp-sp-splendid. Thank you.’
I tried to remember what I knew about Henry Hill Hickman; not much except that he had been the first person to anaesthetise an animal by giving them a gas to breathe and that it had been carbon dioxide, had it not? I lifted my copy of Modern Practice in Anaesthesia off the shelf. The chapter on the history of anaesthesia had been written by Dr Marston, the senior anaesthetist at Guy’s when I had been a student there.
I ran my eye down the page looking at the names. Joseph Priestley... prepared and described nitrous oxide 1777... Davy... born 1778... the famous sentence about nitrous oxide in 1800, and, ah yes, here it is:
It is interesting to note that in the same year Henry Hill Hickman was born, and he did much to forward the possibility of attaining inhalation anaesthesia. It seems that even as a schoolboy Hickman was appalled by the tragedy of unrelieved operative pain, and for this reason he decided to become a medical man. In due course he proceeded to Edinburgh, and as a student witnessed the sufferings of patients in the operating theatre, and decided that he would do his very best to devise some method of abolishing operative pain. He became a member of the Royal College of Surgeons of England in 1820, and commenced his career as a general practitioner in the town of Ludlow.
Ludlow, eh? I still could remember my own daily visits to Ludlow in 1940 when I had been in the nursery class at the girls’ school, before they had sent me away to boarding school. I had always liked Ludlow with its pretty black and white timbered houses and its splendid castle and river. Mother had ocasionally taken us to the tea shop for hot buttered crumpets, though, of course, the 'butter' had been that revolting margarine that we were given during the war.
During the next four years he carried out a number of experiments on small animals, who were rendered free from operative pain by the inhalation of certain gases. The exact nature of the gases inhaled is not definitely known, for although carbon dioxide was chiefly used, it has also been suggested by some historians that the nitrous oxide used by Humphry Davy was also exhibited.

Photo by Janet Quinn, April 2000
18 Teme Street, Tenbury, where Hickman carried out his experiments. It is now a restaurant.
I had not heard about the possibility that Hickman had used nitrous oxide before. I was sure that Alfred Lee in Synopsis of Anaesthesia, which was the book that I had read the most often, had only mentioned the carbon dioxide. It was true, of course, that carbon dioxide would not have produced the same sort of unconsciousness that is produced by conventional anaesthetic agents, for ‘carbon dioxide narcosis’, as is seen in cases of respiratory failure, is due to a change in the acidity of brain cells and fluids. In contrast true ‘anaesthesia’ is due to the action of an anaesthetic agent which occurs whatever the acidity is doing. Still if there had not been too many cardiac arrythmias from the high CO2 level it would presumably have worked just as well in removing the pain of surgery. Why only last week I had put an endotracheal tube down a woman with severe asthma, whose CO2 tension had been 120 mm Hg at the time, and I had heard the sound of some of the turbinate bones cracking as I had pushed the tube through her nose; she had not reacted to this at all. It must have been just like a Henry Hill Hickman’s experiment Well, not really, of course, as the patient had become unconscious from her own carbon dioxide rather than being given some to breathe by an outside party. I continued reading:
According to Hickman the animals were definitely rendered unconscious and free from pain by an inhalation technique, and this discovery was a further progress towards the gaol of anaesthesia. Unfortunately, this fact was not recognized at the time, for when Hickman read a paper before the London Medical Society in 1824, his views were received with apathy and considerable opposition.
Poor Hickman. That must have been immensely frustrating for him. Fancy their not appreciating what an amazing thing he had done.The next paragraph was about his unsuccessful attempt in 1828 to interest the French Academy of Medicine in his work.
... thoroughly discussed, but, alas, the French physicians were not impressed by Hickman’s views and declined to pursue the matter any further.These events were, indeed, a sad disappointment, and Hickman returned to his native land much depressed by his failure to secure interest... died on 5th April 1830, at the early age of 29 years. He was interred in the churchyard at Bromfield, and 100 years later his tomb was restored by the Section of Anaesthetists of the Royal Society of Medicine, and a tablet erected to his memory in the adjacent church.
Good gracious, thought I, Bromfield was only seven or so miles from Brimfield where Janet and Sheila and Mother and I had spent those early war years. We had never actually been to Bromfield at that time, as far as I could remember, but I vowed that one day I would go there to see the grave and the plaque.
Brian and I were talking about Oxygen Therapy to the 5pm meeting in the postgraduate centre. When I thought of all the effort that I had put into preparing it, I felt highly aggrieved by the poor attendance. Brian, of course, was speaking about oxygen therapy in neonates, while my brief was the adults.
One of the physicians asked:
‘Does this hypoxia really matter? I mean many patients are moderately hypoxic for years and yet they seem to manage.’
I groaned inwardly. How were we to get our oxygen therapy right when the Old Guard were asking questions like that?
‘I am not talking about chronic disease here, only acute illnesses where there is acute hypoxia. And yes, it does matter. You see patients in the ITU who will produce urine satisfactorily if their arterial oxygen tension is kept above 9, for example, but who stop producing urine if it falls below 8. And as Haldane said in 1917 anoxaemia not only stops the machine it wrecks the machinery![1]
Now that I had moved ‘sideways’ at Southmead, i.e. was now employed by the Health Service rather than the University, I had in my contract one ‘notional half-day’ a week (three and a half hours) for work on the ITU. In essence this meant that I looked in on the ITU every day of the year, including Saturdays and Sundays, unless I was on holiday. Of course the ITU was not always busy, though often it was, and with six operating lists and a whole day on the labour wards as well, plus my share of the emergency work, the week was a pretty full one. As it happened I was not the first person to have a session allowed for work in the ITU. There had been one such session in the original job plan of an appointment in 1974, but as the succesful candidate had opted to go ‘maximum part-time’, he had dropped it even before he started in post. In the meantime James had carried on selflessly providing the main cover for the Unit without any formal recognition or reward at all.
One day David phoned when I was with a patient in the recovery ward.
‘John, could you look at a young lad in the orthopaedic ward. He broke his femur yesterday and they fixed it in theatre nail last night. He seemed a bit blue this morning so they measured his blood gases, and his PaO2 was only 48; they’ve put him on forty percent oxygen, but he doesn’t seem any better.’
‘Yes, of course. Sounds like fat embolism, doesn’t it?’
I picked up a 60% oxygen mask as I left the recovery ward, and we went together to see the sixteen year old boy. He was clearly not at all well; his face was ashen pale with a blue tinge to his lips. He was not obviously breathless at rest, but he could not finish a sentence without gasping in the middle of it. I changed the mask and we moved him down to the ITU. His PaO2 was still below 50, so I gave him 100% oxygen by what we always called a ‘Water’s circuit’, but which was really a Mapleson C system.
‘Sister, could you get a Cape* ready, please? And, David, get me some Valium and some Phenoperidine. Oh, and some Alloferin too. Thanks.’
I explained to the young patient that I was going to give him something to make him sleepy and that when he woke up we would be helping his breathing with a machine. David brought the drugs I had asked for, and, just before I gave them, he took yet another sample of blood. By this time the skin and tissues over both his left brachial and radial arteries was beginning to look very bruised and swollen from the repeated needle punctures.
Once I had sedated and relaxed him, I put a tube down through his mouth and found he was easy to ventilate.
‘I’ll change this for a nasal tube now while he is still heavily sedated and before the relaxant wears off,’ I said. ‘It will be easier to manage than an oral one, and it avoids the tube and the tape pulling at the corner of his mouth like a horse’s bit.’
I did this and we settled him on the ventilator. He did not look much better, and his PaO2 had only risen to 56mm Hg.
‘We’ll try some PEEP,’ I said. ‘That may help.’ And then, ‘I hope it does; I don’t know what we will do if it doesn’t.’
‘What’s PEEP?’ asked the staff nurse who was helping us, but who was new to the ward.
‘Oh, positive end-expiratory pressure, ‘ I replied. ‘It keeps the lungs expanded and stops the airways closing. It sometimes helps a lot.’
So we got the Cape PEEP valve from the cupboard and placed it between the end of the expiratory tubing and the machine.
‘Let’s set it so that the pressure doesn’t fall below 5 cm of water. There, that’s about it. Am I deceiving myself or is he looking pinker already?’
But there was no doubt about it. His previously blue lips were now definitely pink, and even as we watched the ashen pallor of his cheeks began to change as well, as though at last there really was some blood flowing through his tissues. When we measured it, his PaO2 was 110 mm Hg.
‘We’ll be able to lower his inspired oxygen a bit, thank heavens. I never like these very high concentrations. There was an interesting article by Nunn and some others whose names I forget[1] in the BJA a few years ago, on the use of iso-shunt lines to help you decide how much oxygen to give. We ought to have a copy of it here in the ITU. Anyway for the moment let’s see what happens if we drop to 80% oxygen.’
The PaO2 fell to 73, which was OK. We plotted the various values on a piece of paper and pinned it on the wall:
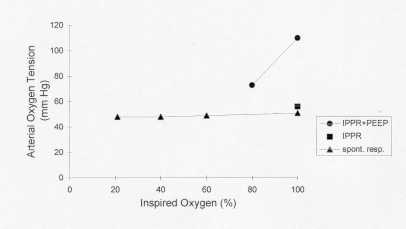
‘That looks just like the chart in Nunn’s paper,’ I said. ‘Aren’t they clever folk at Northwick Park?’
‘Yes,’ said Julia, the Sister-in-charge. ‘But I expect they are not so good-looking.’
‘You could be right,’ I replied.
‘When did PEEP come in use?’ asked David.
‘Oh, well, that depends exactly what you mean by ‘come into use’. When I started anaesthesia in Taunton in 1959, all the patients got PEEP. The consultants used to tighten the expiratory valve so that there was a loud whistle each time the patient breathed out. I remember Arthur, the registrar, saying that the old fools didn’t realise that the increased pressure would dam back the blood from the right side of the heart. What he didn’t realise, and nor did they, was that they were increasing the patient’s FRC and possibly improving their oxygenation, even though they were doing it merely to help them keep track of their patient’s respiration. But, now I come to think of it, the oldest consultant did say once that he though the increased pressure helped keep the patient’s lungs expanded, so perhaps he was a wiser old bird than the registrar appreciated.’
‘1959, eh? That’s almost twenty years ago now. I meant when did people start using PEEP to improve oxygenation in patients on ventilators.’
‘Well, strangely enough the first paper that showed a rise in PaO2 if some PEEP was applied was in 1959. Some people from New York, I think. I’ve never actually read their paper[2], but everyone quotes it. Then in the early sixties, the people in Boston, including John Hedley-Whyte, who was a student at Cambridge with me, showed that there was a progressive fall in PaO2 during anaesthesia [3,4] and that this could be reversed by a few big squeezes on the anaesthetic reservoir bag. So we started giving all the patients on ventilators two or three ‘sighs’ every hour. Then Nunn, in a paper[5] in the BJA in 1964, showed that it didn’t work during his anaesthetics. He applied a pressure of 40cms of water for 40 seconds, and though this made the pulse disappear at the wrist, it didn’t change the oxygen tension. But, of course, these were people with normal lungs. In the late sixties there were several papers about, but as far as I am concerned it was not until I read Keith Sykes’ book on respiratory failure[6] that I realised there really was something in it. Which reminds me, there is a new edition out; I must get myself a copy. Also there was an excellent review[7] of PEEP in one of the surgical journals few years ago by David Ashbaugh, who was in Denver when I was there. Why don’t you look it up? I would like to read it again, if you manage to find it.’
‘OK, I’ll do that. Anyway, PEEP seems to have helped this young man.’
‘Yes, it does.’
We were able to take him off the ventilator a few days later, and he made a good recovey from his fractured leg.
It was good to have a change. I had agreed to take on an in-patient dental list each Thursday morning. I was actively looking forward to getting to grips with nasal intubation once again on a regular basis, instead of just occasionally when we had a mixed parotid tumour to excise, a salivary calculus to extract or an infant with epiglottitis. I knew that James was rightly considered the expert at ‘blind’ nasal intubation at Southmead now that Terence had retired, and that he relied heavily on getting the patient’s head into the optimum position and making him overbreathe by giving him high concentrations of carbon dioxide (up to 16%). He had been taught by none less than the redoubtable Tom Boulton of Reading, so he was certainly well schooled. For myself I had always felt that, in my hands at least, there was still a failure rate with ‘blind nasals’, and these occasions were sometimes fraught with problems like laryngeal spasm and nosebleeds. Although I enjoyed the challenge I considered that I was still looking for a totally foolproof method. I thought that blind nasal intubation often was easier in the relaxed patient, or perhaps it was because it was so much quicker than taking them deep with an inhalational agent that it just seemed easier. I remembered many years previously discussing it with Terence, who had said quite uncompromisingly
‘I think that anybody who gives muscle relaxants to a patient for taking a few teeth out must be mad. What is wrong with simple old-fashioned surgical anaesthesia? Anaesthesia is like marriage, you know, an honourable estate ordained by God. Why on earth would you need to stop the patient from breathing just to take a few teeth out?’
Well, that was one way of looking at it, but I still thought that the advantages of relaxants outweighed the advantages of nostalgia.
After a few weeks, and scores of wisdom teeth, I had settled into a routine using alcuronium to relax the patient, so allowing myself the luxury of good intubating conditions without the risk of muscle pains. It did make it necessary, of course, for me to ventilate the patient during the surgery. This had certain advantages at the end of the operation as extubation from a relaxant based technique was consistently more satisfactory than when relaxants had not been used.
One day a young Malayan registrar who was working with me for the morning found that however hard he tried he just could not get the tube to go down the trachea, yet when I tried I had very little trouble.
‘I have just cottoned on to why I got the tube down when you were having so much trouble,’ I said. ‘Having got the tube in the midline, and behind the epiglottis, under direct vision with the laryngoscope, I let the various bits of anatomy fall back into their normal positions before I pushed the tube forwards. In contrast, you were trying to see the glottis and the more you lifted it into view, the more difficulty you had because you distorted the anatomy and the trachea was no longer in a straight line with the tube. Clearly, the thing is to pass the tube blindly once you have placed it optimally under direct vision.’
I have used and demonstrated this technique many, many times. It has always (well nearly always) worked like magic.
No one liked working in B block; ‘the blue walls make all the patients look blue’ was the common complaint. The sense of ill ease this created was not helped by the Manley ventilator which suddenly malfunctioned one day, or at least appeared to malfunction. Kay was giving a routine anaesthetic when the patient had suddenly gone blue. Of course, she had immediately turned the oxygen up and switched over to squeezing the anaesthetic bag by hand instead of the using the ventilator and everything had got better in an instant.
‘I’m not sure exactly what happened but I can only assume that something went wrong inside the ventilator,’ she said. ‘Luckily it all came right when I switched over to hand ventilation and the patient didn’t come to any harm, but it certainly didn’t do my coronary arteries any good.’
She sent for the engineer and he stripped the ventilator down but found nothing wrong with it.
‘I am sure it was the Manley,’ Kay insisted. ‘A valve must have stuck or something.’
The next day there was another Caesarean section to be done. When I went to see the mother in the ward she said:
‘I would like to have a general anaesthetic, please. I don’t think I could cope with being awake during the operation.’
‘Of course, you can have what you like, but most people do find an epidural very satisfactory even if they are a bit apprehensive about it. But I’m not here to twist your arm if you really don’t want to try it. I haven’t been able to find your notes yet; have you had any problems in this pregnancy?’
‘No, none at all, though I think I ought to tell you that I am very allergic to one of those drugs that they give you for pain, you know, like Pethidine. The young lady anaesthetist came and spoke to me after my last operation and said I should never have any of those drugs again.’
‘Oh, I’ll have to find out what that was all about. I’ll go and look again for your notes.’
Eventually I did find them, filed in the notes-trolley in the wrong folder. I searched through her notes till I came to the previous anaesthetic chart. Ah, here it was. Yes, the arm had become very swollen almost immediately a dose of Fentanyl had been given into a vein. The redness and swelling had lasted for nearly two hours, though her general condition had remained OK. I had often seen local wheals and flares along the course of a vein after Fentanyl or morphine, but this did seem to have been something extraordinarily dramatic. Vivienne, the young anaesthetic SHO who had given the anaesthetic, had drawn a vivid picture of a swollen arm.
Well, that would certainly make things very awkward after the operation, but it sounded as though it had only been a local reaction. Still it would be awkward if she got the same sort of reaction to intramuscular injections as she had to the intravenous one, and she probably would if I used Fentanyl again.
‘I think that what we’ll do is this. We’ll just go ahead in the normal way till the baby is born, and then I’ll test you very carefully with a different sort of painkiller and see how it goes. I’ll just give you a tiny dose at first and slowly increase it. That way we’ll find out if the drug I have chosen is OK for you or not.’
‘Thank you, doctor. That sounds a good idea.’
I hoped that it was Anyway that’s what I did. I decided to use Temgesic as it could be given either by injection or as a small tablet that could be sucked under the tongue.
The following day I gave the lady her anaesthetic as we had agreed. Once the baby was delivered (a splendid boy who yelled the moment he was born) I diluted an ampoule of Temgesic and gave her one ten thousandth of the normal dose; no problem. So I gave a thousandth of the normal dose; again no problem. So next a hundredth, and then a tenth, and then a half dose; no problems. Her pulse rate and blood pressure were steady and there was no local reaction around the site of injection. So naturally I gave her the other half.
It was at this moment that she started to breathe a just a little by herself and slightly move her head. As I wanted to watch her closely just to be sure that she was OK now that I had finally given her the full dose, I turned the nitrous oxide up to 75% from the 66% she getting. I planned giving her a further dose of relaxant in another few moments.
As I watched she started to go blue. Dear God, what on earth was happening? Why was she going blue? I checked that the oxygen was still flowing. Yes, the bobbin was spinning at 2 l/min just as it should have been. I looked at the top of her chest to see if both sides were moving. Yes, they were; I had not pushed the tube down too far so that only one of her lungs was being ventilated. So why was she going blue before my eyes, and getting bluer by the minute? It must something to do with the Temgesic. I felt a cold sweat break out on my forehead and my pulse raced with the adrenaline I was pouring out.
For a few moments I was frozen with horror at the thought that I had done the wrong thing in giving her the wretched drug; then, luckily, instinct took over and I turned up the oxygen.
To my relief she turned a wonderful pink; clearly it was nothing to do with the Temgesic after all. I tried to convince myself that I had never really thought that it could have been, but for one terrible moment I certainly had thought it. Even now I was not clear what had happened.
So that she would not wake up while the operation was still under way, I turned the flow of oxygen down again till I was giving her a mixture of 50% oxygen and 50% nitrous oxide, together with a low dose of halothane. Everything stayed OK.
‘I don’t really understand what went wrong there,’ I said to the obstetrician, ‘but we seem to be back on an even keel, so let’s get the job finished, before anything else disastrous occurs.’
He quickly finished sewing together the different layers on the patient’s abdominal wall, and when he had finished I turned off the halothane and the nitrous oxide and let her wake up.
‘Hello, Mrs Sampson. Can you hear me? You have a lovely baby boy. The operation is all over and everything is fine. I am just going to take that nasty tube out of your mouth. Open your mouth for me. There that’s better, isn’t it?’
She opened her eyes and smiled.
‘A little boy? That’s nice. I was hoping for a boy.’
The midwife placed the baby beside her so that she could see his face and cuddle him. She appeared to be quite free from pain but I did not know whether this was because of the Temgesic or the distraction of holding her baby; both perhaps.
Now, of course, I had to sort out exactly what had happened to make her go blue in the middle of the operation. I put a notice on the anaesthetic machine saying that it must not be used till further notice, and I went off to the Intensive Care Ward to borrow an oxygen analyser.
Twenty minutes later I was testing the gas mixture as it came out of the anaesthetic machine. At first I could find nothing wrong. When I set the flowmeters to give 50% oxygen-50% nitrous oxide that was exactly what I got; and a 25% oxygen-75% nitrous oxide was also correct. But although I was passing the gases through the ventilator it was not switched on. Perhaps it would be different when the thing was working rather than merely acting as a conduit.
I put an anaesthetic bag on the end of the ventilator to act as an ‘artificial lung’ and switched on the machine. With both the flowmeters set at 5 l/min the reading on the oxygen analyser was now 40%, not 50%. I altered the flows so that I should have been getting 30% oxygen but the analyser now only read 25%. I changed the flows once more so that now I should have been getting 25% oxygen. The analyser reading was not quite steady; it varied between 9% and 10% No wonder the lady had gone blue.
Of course, there must be a leak of the oxygen somewhere that was above the bobbin in the flowmeter and before the point where the oxygen mixed with the nitrous oxide. That was the only explanation.
I moved the anaesthetic machine out of the theatre into the corridor covered it with hazard notices and phoned the service engineer.
Next day we tested the machine together. It passed the normal test for leaks, which involved blocking the outlet and pressurising to 40 cm of water and showing that this pressure was held for five minutes.
‘But the back pressure from the Manley is much higher than 40 cm of water,’ I said. ‘I measured it yesterday and it was 18 kilopascals which is several metres of water, not just 40 cm.’
‘But you normally don’t use pressures higher than 40 cm of water to ventilate patients, do you?’
‘No, we don’t. But now you are talking about the pressure on the patient side of the Manley. I am talking about the pressure on the machine side. Your test would be all right for ventilators that don’t rely on the gas pressure to work them.’
‘Well, let’s strip the machine down and see if we can find the leak.’
We found it at the top of the oxygen flowmeter. There was a circumferential tear in the rubber seal that you could not see unless you pulled the edges apart. Clearly it was not producing any significant loss of oxygen when the pressure was low. It was only back pressure from the Manley that caused a problem.
That afternoon I got the hospital photographer to take a photo taken of the seal while I displayed the tear by pulling it open. I sent it with a letter to the British Journal of Anaesthesia, which is how a picture of my left thumbnail[1] came to be sent all over the world.
'Isabel, you know that I have this bee in my bonnet about the position you should put a newborn baby in when it's delivered by Caesarean section. Well, I'm going to write to the Lancet about it.'
'Good. I'm glad that you are. I remember you're telling me about it. Not leaving them flat on their backs, as they can't always get rid of the fluid in their mouths and throats if you do. That was it, wasn't it?'
'Yes, that's right. In the old days the obstetricians used to hang the baby upside by its feet for a few moments to let the fluid run out. These days it's thought that this can increase cerebral oedema or cause intraventricular haemorrhage and also it may hinder the baby breathing by the pressure of the abdominal contents on the diaphragm. All that may well be true, but at least the fluid drained out.'
'Yes, I saw them do that way at Guy's in the fifties. What do they do these days?'
'Well, often the surgeon places the baby on its back on or between its mother's legs while he delivers the placenta or cuts the cord. After that the baby will often be carried across the theatre on its back and then be placed, still on its back, on the resuscitation trolley. Most babies cope perfectly well with this, but every so often there's a baby that doesn't clear the fluid from its throat.'
'What happens then?'
'Well, it may breathe OK at first but then it starts to gargle, and sooner or later it stops breathing. This may be because the fluid sets off a reflex - you know, the same sort of thing that happens if you stuff a suction catheter too deeply in to the throat - or it may obstruct the airway with foam.’
‘Foam?’
‘Yes, foam. Fifteen years ago a South African called Klein wrote to the Lancet about babies foaming at the mouth some minutes after delivery[1]. Of the twelve cases he reported, eleven were born by Caesarean section. He thought it was due to lack of chest compression during birth, and consequently an excess of foetal lung fluid when breathing began. He may be quite right, of course, but unfortunately he does not say into what position the babies were put after delivery, so we can’t say whether this fluid was given the chance to drain effectively. My guess is that he was talking about the same sort of thing as I am.’
‘Don’t they sometimes hold the baby up, in a sitting or standing position, so that the mother can see them just after they are born?’
‘Yes, they do. It may well be that this is a good thing, as it makes it easy for the babe to spit out or swallow any excess fluid. Certainly it is another way of not letting it lie flat on its back.’
A few days later I did get a short letter off to the Lancet, and to my delight they agreed to publish it. A couple of weeks later I went to the library to see if the new journal had arrived. Yes, it had, and, yes, the letter was there all right, but, just look at this, in the list of contents on the front cover they had given me the title of 'Professor'! I laughed out loud. One or two people looked up from their books, wondering what had on earth was going on. Quickly I turned the letter pages. No, they had not given me the wrong title on the letter page itself. Thank Heavens for that! It would have been most embarrassing, but I could live with a misprint at the front of the journal. I wondered how it had come about. Professor, eh? Sounded quite nice really. Perhaps they had confused me with Peter.
I was expecting a flurry of comment in the next few days, but none came. There were no replies in the correspondence columns of the Lancet, nor any comment from my medical colleagues. I was amazed - it had seemed so important to me, and so ripe for discussion.
So I was pleased when some weeks later Nursing Times ran a small article about my letter with a coloured picture of a new baby alongside it. In their article they had used my exact words, but had changed the order of the sentences around a bit so that it looked like comment rather than copy. I guess that sort of thing is always happening. Later the Midwifes’ Information Resource (about which I had never heard before) wrote to me and asked if they could reproduce my letter in their monthly handout. Of course I was delighted.
Some months later there was new research published about cot deaths suggesting it was best to leave babies on their backs at night. As I felt this was an entirely different story, I hoped that it would not confuse the message I had been trying to put across.
It was Monday morning. We were slowly gathering together in the Seminar Room for the departmental meeting.
'Before we start,' said Neville, who was standing up at the front of the room, looking slightly mischievous, I thought, 'I have a new question for the Final Fellowship exam. You are in the ITU when without warning both the piped oxygen and the electricity fail, and what's more the emergency generator also fails. What do you do?'
A brief pause and then someone, I can't remember who it was, started to chatter about Ambu bags and oxygen cylinders, but Neville cut him short.
'Oh, you will have to say all that, of course, but there is only one answer that will get you through the exam.' He paused for effect. ' It's simple really. You just have to arrange that Alun Jenkins is on duty. That's all. He will sort out everything for you.'
He went on to describe how just such an incident had arisen over the weekend and how effective and efficient Alun had been in producing cylinders and other vital equipment. It had been quite a picnic, but happily none of the patients had come to any harm. Well done, Alun!
'Iain, it will 40 years next September since the Clevedon ventilator was first used. We really ought to mark the occasion somehow.’
‘Yes, that’s a good idea. Where is the Clevedon now?’
'Oh, when they closed Ham Green hospital in 1989 I took it over to the Monica Britton Exhibition Hall at Frenchay, but I think it is just in a cupboard getting dusty. If I got it back I thought you could get it going again while I wrote up something about it.’
The Clevedon ventilator, Nov 1993
The Clevedon was the very first positive pressure ventilator to be used in the South West of England. It was a fascinating story. Following the development of a ventilator by Bang[1] in Denmark in 1952, Dr. Macrae and his colleague Dr. Walley teamed up with an engineering firm in Clevedon, the Willcocks Co, and together designed and built one themselves. They called it the Clevedon Respirator[2]. It was a splendid machine. The first patient on whom it was used was a young man of twenty-one who was admitted to Ham Green hospital on September 23rd 1953 with severe poliomyelitis[3]. He was ventilated for six weeks and then made an excellent recovery.
Iain and James and I had first met him in 1979 when he had been in our Intensive Care Unit with chest problems, which were largely because his cough was too weak to clear his sputum properly. He was back in the ITU again twice in the next two years, and eventually it became clear that not only was he not coughing well, but that at night he was seriously underbreathing.
'When he goes to sleep his carbon dioxide level is higher than his oxygen level - a classical case of Ondine's curse[4],’ said James.
It was the sort of thing that we saw more commonly in the recovery ward if a patient had too much morphine on board.
'We may have to send him home with a permanent tracheotomy and give him a ventilator to take with him for when he wants to go to sleep, ' James continued.
'We should get Ron to see him,’ said Iain. 'He may have some suggestions.'
'That’s a good idea. I'll give him a ring,' I said.
In the end we had sent the patient home with an uncuffed silver tracheotomy tube in place and an East Radcliffe ventilator, which had to do until we could get something more suitable. I went to see the hospital secretary, Mr Archer, who was most helpful. He told me to go ahead and buy what we needed and to let him have the bill. He would sort it out somehow. The ventilator we bought was a Cape minor T50. The patient had got on extremely well over these last 12 years, connecting himself to the Cape at night-time, and during the day blocking the silver tube off, hiding it behind collar and tie.
A few days after my conversation with Iain I motored across to Frenchay to collect the Clevedon from the Monica Britton Hall. It seemed amazing to me how intertwined were people’s lives. It was Monica Britton, in whose memory the Hall had been built, who had funded Katy and the other girls from Colston's school to go on the Outward Bound in mid-Wales more than twenty years ago.
When I got back to Southmead I delivered the ventilator to the Urology Theatres for Iain to sort out, with Jim’s help no doubt, when he had time.
Next morning I went to the library of the University Department of Community Medicine at Canynge Hall in Whiteladies Rd. I searched through the Annual Report(s) of the Medical Officer of Health, City and County of Bristol, and also old copies of the Bristol Medico-Chirurgical Journal, in which there were three reports on Poliomyelitis in Bristol by Dr Macrae (1947, 1950 and 1954).
It took me a couple of hours to get the figures I needed. When I got back to the hospital Chris plotted them out for me on the computer and we compared them with data from England and Wales from 1930 which I had gathered previously from reports in the Medical Annual, the Lancet and the BMJ.
The first wave of poliomyelitis that had swept the country during the long hot dry summer and autumn of 1947 had only lightly affected Bristol. Incidentally this was just a year or two after large numbers of troops had returned to the UK from the Far East where poliomyelitis was endemic. Thereafter the peaks and troughs in Bristol roughly followed those in the country at large. The Salk (killed virus) vaccine had been introduced in 1956 and the Sabin (live attenuated virus) vaccine in 1962. They had been remarkably effective.
So far so good, but I decided that I needed more information. I went to the University library and browsed through Illustrated History of Medicine by J-C Sournia, a splendidly informative and beautifully illustrated book (London: Harold Starke, 1992). Then I moved on to History of Poliomyelitis by JR Paul (Yale University Press: New Haven and London, 1971). From these two books I learned amongst many other things that
poliomyelitis was a disease of great antiquity – one had a picture of a Egyptian priest carved on a stele from the eighteenth dynasty, i.e. 1580 -1350 BC, who had a withered and shortened leg with the foot held in the typical equinus position of flaccid paralysis. Poliomyelitis is the most likely cause[5].
the earliest case on record in the British Isles was Sir Walter Scott, b. 1771, who said: at the age of eighteen months had had a febrile illness and had lost the power of his right leg[6].
the disease was first described in the medical literature in 1789 by a doctor called Underwood[7].
the word poliomyelitis comes from the Greek polios, grey, and myelos, marrow.
the change from endemic to epidemic disease that occurred in the latter part of the nineteenth century was probably the result of improved hygiene, because children were no longer routinely being exposed to the virus while they still had passive immunity from their mothers.
the poliovirus was discovered in 1908.
poliomyelitis became a notifiable disease in the UK in 1912, following three small outbreaks in the South West of England in 1911.
I phoned the patient, now sixty-one years old, and asked him if I could come round and take a photograph of him. When I got to his house I found him in good spirits. He took me upstairs to see the Cape, which was covered with stickers of the French towns he had visited on holiday. I explained what I was doing, and asked him if he wanted his name mentioned or not.
‘Just call me by my first name’ he replied. ‘That’s how everyone knows me.’
The photos came out very well. I told Iain how I was getting on.
‘Well, I’ve got the Clevedon working again. Come and see. It’s in the corridor outside Urology theatre 2.’
When we got there he plugged it into the electricity while Jim connected it up to a gas supply and put a reservoir bag at the far end to act as a pair of lungs. With a flourish Iain switched the machine on. I watched with fascination as the air pressure increased inside the machine, the water levels changed and the tilting mercury switches sparked. I had forgotten what a wonderful sight it was. The last time I had seen a Clevedon working it had been at Ham Green in 1964, when Fen had arranged a visit there for the registrars in the department. This was the year before the ITU was opened at the Infirmary.
‘The Ancient Greeks would have liked this,’ I said. ‘What a grand combination of fire, air and water! Are you going to use it on a patient?’
‘No,’ he replied. ‘I don’t think it is reliable enough to do that, which is a pity. Ted Nesling had a working Clevedon in his anaesthetic room at Plymouth up to a very few years ago, but that one was carefully maintained, while this one has been horribly neglected. Incidentally do you know how many Clevedons were made altogether?’
‘No, I don’t. I must find out if the company that made them is still in business.’
I looked in the phone book and discovered that was it. I had an interesting chat on the phone with the manager. He told me that the original Mr Willcox had been heavily involved in building cars for Henry Segrave when he broke the world land speed record, and that about thirty Clevedons had been built in all, some of them being sold to hospitals in Ireland.
When Ham Green Hospital had been closed in 1989 someone had saved the old notes from the 1950s, which were bound together in heavy leather tomes and brought over to Southmead. I had been was fascinated then to read the original case notes when the Clevedon had gone into service for the first time, and I dug the notes out again.
Now I wanted to find out more about the Copenhagen epidemic in 1952, which saw the birth of intensive care in Europe. I read Lassen’s account[8] of the epidemic. It was quite staggering. From the beginning of August till the end of the year 3000 cases had been admitted to the Blegdam hospital; 2241 of these had been confirmed as poliomyelitis; 1250 had some paralysis; 345 of these needed special treatment for respiratory insufficiency and/or impairment of swallowing. Lassen wrote:
It is doubtful if any city the size of Copenhagen has ever experienced an outbreak of similar magnitude ... for many weeks we received thirty to fifty patients daily, of whom six to twelve were desperately ill ... drowning in the own secretions. As we felt that the application of modern principles of anaesthesia to the problem of obstructed airways and respiratory insufficiency in poliomyelitis might improve our results anaesthetists were invited to join our staff, the first of these being Dr. Bjørn Ibsen.
Bjørn Ibsen
Dr Ibsen[9] was called into consultation on August 25th. In the preceding three weeks there had been 31 patients with life threatening poliomyelitis; 28 of these had died. On August 26th the first patient was treated with the method that was to become the treatment of choice[10]: tracheotomy just below the larynx, an inflatable rubber cuffed tube in trachea, frequent suction, repeated bronchoscopy postural drainage and manual positive pressure ventilation using oxygen and nitrogen. The apparatus used for ventilating these patients was amazingly simple, consisting of a Waters cannister filled with soda-lime for absorbing carbon dioxide and a reservoir bag which was squeezed by hand.
Copenhagen 1952
from Lassen HCA. Management of Life-threatening Poliomyelitis. p.63. E & S Linvingstone, Edinburgh & London, 1954.
At times there were as many as 70 patients requiring artificial respiration. Students from the University provided the handpower. Overall 1400 students were involved during the course of the epidemic. None of them contracted the disease. By the end of the year the mortality in these severe cases had fallen from 87% to 26%.
And so I assembled my small pamphlet, and placed it with the Clevedon ventilator on a table in the medical library at Southmead. I left them there for two weeks before taking them to the museum at Frenchay.
NOTES
[1] calculated from birth weight 3.5kg, oxygen consumption 5ml/kg/min and respiratory quotient = 1.0 (strangely, the respiratory quotient is 1.0 during the first 24 hours after birth, rather than the normal 0.8.)
1939
[1] an emulsion of benzyl benzoate for the treatment of scabies. This emulsion is still available in the UK, but not the USA or Canada.
[1] Valsalva actually described his manoeuvre as forced expiration with an open glottis against a closed mouth and nose, so that pressure was exerted down the Eustachian tube.
[1] An old fashioned Bilroth 1 partial gastrectomy. My mother had already had ten years of medical treatment for her duodenal ulcer, which consisted of taking antacids and living on a bland diet, such as white fish poached in milk. She also took milk and biscuits to bed with her, so that she could have something every few hours throughout the night. She did not have her curative operation until she had had two massive haematemeses, and the operation took four hours, as it was technically difficult because of the fat she had laid down while on her milky diet. Her surgeon was Grant Massie, who, coincidentally, lived in the very house that my father had lived in at the start of the First World War. The Bilroth 1 was a very satisfactory operation when it was successful, as it was for my mother, but post-gastrectomy syndromes ruined the lives of a small percentage of patients.
[2] I suppose it was no worse than taking her a jam jar containing two copulating frogs; I had done this once when visiting her in hospital after one of her haematemeses.
[1] I have changed my mind about this. In June 1998 I was admitted to hospital with Salmonella septicaemia after eating an egg bought from a canal-side shop. Come back Edwina!
[1] I said this to George Wilmot once. He replied ‘It didn’t work! I was there on day one, and I never saw so many people being sick.’
[1] Later to become Bristol's first professor of anaesthesia.
[1] Marshall BE, Millar RA. Some factors influencing post-operative hypoxaermia. Anaesthesia. 1965;20:408-428.
[1] Geoffrey wrote three classic papers about his experiences with these cases: Burton G W. Metabolic acidosis during profound hypothermia. Anaesthesia 1964; 19: 365-375; Burton G W, Holderness M C. On the management of massive blood transfusion. Anaesthesia 1964; 19: 408-420; Burton G W The value of carbon dioxide monitoring during anaesthesia. Anaesthesia 1966; 21: 173-183. See also my comments in Anaesthesia in the Sixties - Bristol fashion.
[1] Cormack R, Powell JN. Improving the performance of the infra-red carbon dioxide meter. Brit. J. Anaesth. 1972; 44:131-141.
[1] Haldane JS. Brit. Med. J. 1917;1: 181. I have always liked this splendid adage. In later years I have tended to make the same point by asking why is oxygen more like oil than petrol?
[1] Benatar SR, Hewlett AM, Nunn JF. The use of iso-shunt lines for control of oxygen therapy. Brit. J. Anaesth. 1973; 45; 711.
[2] Frumin MI, Bergman NA, Holaday DA, Rackow M, Salanitre E. Alveolar-arterial O2 differences during artificial respiration in man. J. Appl. Physiol. 1959; 14: 694.
[3]Bendixen HH, Hedley-Whyte J, Laver MB. Impaired oxygenation in surgical patients during general anesthesia with controlled ventilation. New Eng. J. Med. 1963; 269: 823.
[4]Bendixen HH, Bullwinkel B, Hedley-Whyte J, Laver MB. Atelectasis and shunting during spontaneous ventilation in anesthetised patients. Anesthesiology. 1964 ; 25; 297.
[5] Nunn JF, Bergman NA, Coleman AJ. Factors influencing the arteriasl oxygen tension during anaesthesia with artificial ventilation. Brit. J. Anaesth. 1965; 37: 898.
[6] Sykes MK, McNicol MW, Campbell EJM. Respiratory Failure. Oxford: Blackwell Scientific Publications, 1969. I bought the second edition (1976) a few days later; it was my standard reference in the ITU for many years.
[7] Ashbaugh DA, Petty TL. Positive end-expiratory pressure: physiology, indications and contra-indications. J. thorac. cardiovasc. Surg. 1973; 65: 165.
[1] It was this thumb nail that later got infected with yeast - see chap 11/1989 and 90a.
[1] Klein M. Asphyxia neonatorum caused by foaming. Lancet 1972; I: 1089-91. In August 2004 I had an e-mail out of the blue from a Max Klein asking where he could find a picture of the East-Radcliffe ventilator. Of course I asked him if he was the Max Klein I had referred to in my letter to the Lancet in 1987. He replied that he was, and how he too had been surprised that there was so little response from his own letter 15 years earlier, which he had thought was important. A few days later I showed this email correspondence to my friend Peter Dunn, while we were playing chess. Peter said I was quite wrong about the foaming babies, and that it was due to early cord clamping in babies who had a lung full of fluid by not having been through a period of labour. This, he said, occurred particularly after elective Caesarean section. Normally the surge in catecholamines during labour causes resorption of much of this fluid. Additionally, the vaginal squeeze of the baby's thorax during normal delivery causes further evacuation. After elective Caesarean section with a lung still full of fluid, the pulmonary vascular resistance remains high and with the clamping of the cord and the cutting off of the low resistance placental circulation, the baby's systemic blood pressure also rises rapidly. The heart is now beating against two high resistances and may well go into transitory heart failure. The exudation of plasma not only destroys the surfactant but also displaces it up the airway. Hence the foaming when the babies begin to breathe. As he had been writing about this subject for more than 30 years, I am convinced. Perhaps I should not have mentioned the foaming babies at all but should just have stuck to the gargling ones, where I still think my arguments are valid.
[1] Bang C. (1953) Lancet, i, 723
[2] Macrae J, McKendrick GDW, Claremont JM, Sefton EM and Walley RV. (1953) The Clevedon Respirator. Lancet. ii, 971
[3] Macrae J, McKendrick GDW, Sefton EM and Walley RV. (1954) Positive-Pressure Respiration - Management of patients treated with Clevedon Respirator. Lancet i, 21.
[4] Ondine, a water nymph in German legend, took away the reflex nature of her unfaithful husband's respiration so that he had to remember to breathe. When eventually he fell asleep he died.
[5] Hamburger 0 (1911) A case of infantile paralysis in ancient times, Ugeskr. f. laeger., 73:1565.
[6] Lockhard JG (1837) Memoirs of the Life of Sir Walter Scott, Bart, vol. 1, Carey, Lean and Blanchard, Philadelphia.
[7] Underwood MA (1789) A Treatise on the Diseases of Children with General Directions for the Management of Infants from birth. Matthews, London.
[8] Lassen HCA. (1954) The Epidemic of Poliomyelitis in Copenhagen, 1952. Proc. Roy. Soc. Med.47:67, and Lassen HCA. Management of Life-threatening Poliomyelitis. E &S Livingstone, Edinburgh and London 1954.
[9] See Chap 11; 1990b for when I met Dr. Ibsen.
[10] Bjørn Ibsen. (1954) The anaesthetist’s viewpoint on the treatment of respiratory complications in poliomyelitis during the epidemic in Copenhagen, 1952. Proc. Roy. Soc. Med.47:xx.
email john@johnpowell.net